14 Common Causes Of Chest Pain
A stubbed toe — a common occurrence, but an extraordinarily painful one. Minor injuries like this are a painful nuisance but are a regular part of life. But what if you awoke to a squeezing sensation in your chest or felt pressure building behind your breastbone during a workout? For many people, these sensations are cause for serious concern.
This heightened awareness of sensations in the chest is not unwarranted. Heart disease is estimated to kill 695,000 Americans every year, according to the Centers for Disease Control and Prevention. As we age, the risk of cardiac complications and diseases tends to increase, too.
While chest pain is undoubtedly a scary symptom, it isn't always related to the heart. And while chest pain should be taken seriously and always merits medical attention, there's a multitude of explanations for why pain in the chest can occur — some serious, many not.
Heartburn
Some people are surprised to learn that heartburn can mimic the symptoms of more serious cardiac conditions like heart attack. But medical professionals are no stranger to this idea. In fact, gastrointestinal reflux disease accounts for 30% of emergency room patients presenting with chest pain, according to a report published in StatPearls. Suffice it to say, whether you think it might be an upset stomach or not, new chest pain should always be taken seriously.
Repeated bouts of heartburn may suggest an underlying disorder called gastroesophageal reflux disease, or GERD. According to the American College of Gastroenterology (ACG), this occurs when the acidic contents of the stomach bubble into the esophagus. While the stomach is built to handle a highly acidic environment, the esophagus is not as well protected. This can lead to a sensation of pain and discomfort in the lower part of the esophagus, which sits in the chest.
GERD is one of the most common gastrointestinal conditions, affecting up to 20% of the population (via ACG). And while popping an antacid can help manage symptoms as they occur, your primary care provider may want to prevent the symptoms from occurring at all. This is because continued exposure to the erosive effects of stomach acid can lead to an increased risk of esophageal cancer. Thankfully, diagnosis is relatively straightforward and there are many inexpensive, over-the-counter medications that can help control the disease.
Hiatal hernia
Simply put, a hernia is the protrusion of gastrointestinal contents, such as the intestines or stomach, into a location where it doesn't belong. Commonly, hernias of all types go unnoticed and do not become a problem until symptoms like pain and discomfort begin to appear.
One common hernia is called a hiatal hernia. This is when the stomach passes through a hole in the diaphragm and comes to rest in the chest, according to the Mayo Clinic. Like other hernias, this usually remains asymptomatic. However, the Mayo Clinic explains that a hiatal hernia may cause acid reflux, regurgitation, difficulty swallowing, and chest pain.
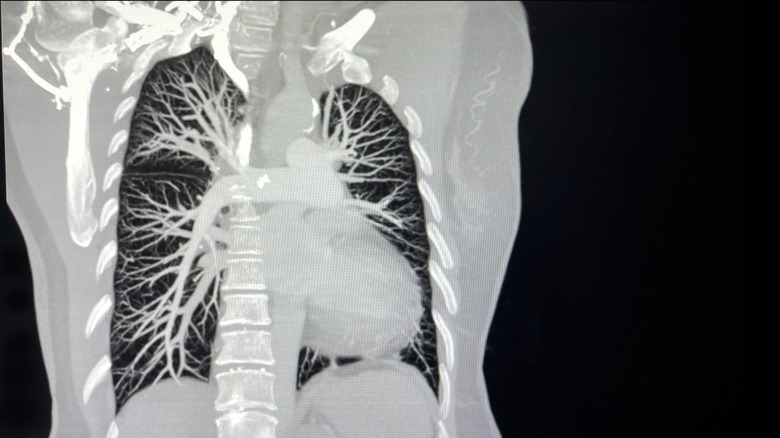
Hiatal hernias are more common with increased age and at unhealthy weights. Further, traumatic injury, surgical complications, or bouts of increased abdominal pressure (such as during weightlifting, coughing, or straining during a bowel movement) may cause this phenomenon. Diagnosis is made with imaging studies such as computed tomography and may require an upper endoscopy. Typically, definitive treatment of a hiatal hernia requires surgical repair to pull the stomach out of the chest and close the hole in the diaphragm (via Cleveland Clinic).
Boerhaave syndrome
The esophagus is the muscular tube that propels food from our mouths down to our stomachs and can be a commonly misunderstood source of chest pain. One of the most dangerous esophageal disorders that can manifest in severe chest pain is called Boerhaave syndrome.
Boerhaave syndrome, described in StatPearls as spontaneous esophageal rupture, commonly occurs after a bout of very forceful vomiting. However, the publication noted, "Other causes include weightlifting, defecation, epileptic seizures, abdominal trauma, compressed air injury, and childbirth." Alcoholism and "excessive indulgence in food" are both risk factors.
Boerhaave syndrome is often suspected when patients exhibit three characteristic signs and symptoms known as the Mackler Triad: vomiting, chest pain, and the presence of air bubbles beneath the skin (called subcutaneous emphysema). However, StatPearls noted that "up to one-third of patients do not present with these symptoms." Further, some patients will exhibit a crackling sound that accompanies the heartbeat when listening with a stethoscope, this is called Hamman's sign.
Boerhaave syndrome is a serious medical emergency that warrants immediate evaluation at the nearest emergency department, and treatment is nearly always accomplished via surgical intervention. Without treatment in 12 to 24 hours, the risk of death is high.
Chest wall syndrome
Chest wall syndrome, also known as costochondritis, is one of the most common causes of chest pain. In fact, chest wall pain accounts for 20% of all patients who present to the primary care offices for evaluation of chest pain, according to the American Academy of Family Physicians (AAFP). The condition usually resolves with time and is rarely dangerous, but any new chest pain warrants evaluation by a medical professional (via WebMD).
Costochondritis, very simply, is an inflammation of the cartilaginous portions of the rib cage. The pain can vary in intensity, but, according to the AAFP, it is "typically described as sharp, aching, or pressure-like" and is "exacerbated by upper body movement, deep breathing, and exertional activities." Furthermore, unlike more serious conditions, the pain of costochondritis can be reproduced by pressing on the affected area, whereas the pain from a heart attack tends to be broad. Treatment for costochondritis can include over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs.
Panic attacks
Those who experience panic attacks know that few things can cause more distress. These intense bouts of physical and mental incapacitation can mimic a few serious conditions, including a heart attack. That is because, according to the Cleveland Clinic, panic attacks include symptoms like chest pain, sweating, trouble breathing, and an impending sense of doom.
However, panic attacks have a few subtle differences that are worth noting. Panic attacks are typically described as a sharp, stabbing sensation whereas heart attacks are commonly described as intense pressure or squeezing. Further, heart attacks tend to occur during or after bouts of exercise whereas panic attacks rarely follow exercise. A panic attack may last "a few minutes or up to an hour," according to the Clinic, and will then resolve, whereas a heart attack only increases or maintains its intensity. Though intensely frightening, panic attacks can be treated with therapy or medication prescribed by a psychiatrist (via WebMD).
Pneumonia
We've probably all experienced a nasty bout of bronchitis, and perhaps an unlucky few have had to endure pneumonia. These illnesses make us feel lousy, and they are a very common cause of chest pain. This makes intuitive sense — the lungs sit within the chest and occupy the majority of its space. Unsurprisingly, according to the American Academy of Family Physicians, "Common symptoms [of pneumonia] include fever, chills, pleuritic chest pain, and a cough producing mucopurulent sputum." Importantly, the AAFP notes that older adults "often present with weakness and decline in functional and mental status." Therefore, if you notice a swift change in a loved one's mental status, it is a good idea to consider that infection may be causing atypical symptoms.
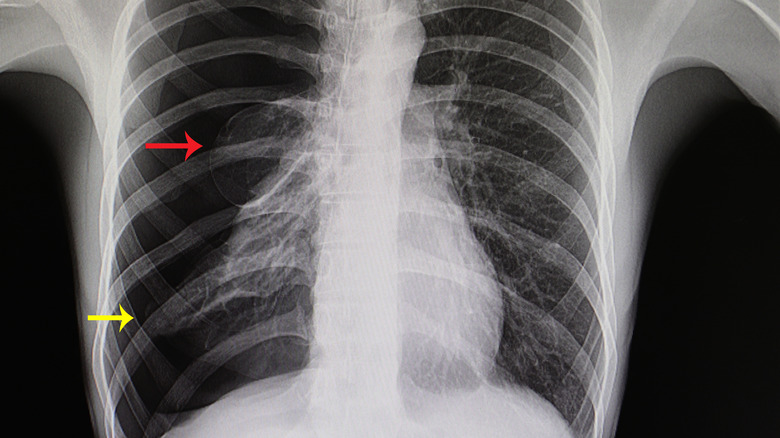
Respiratory infections may be diagnosed without the need for any blood tests or imaging studies. However, in order to assess for pneumonia, your doctor may order a chest x-ray. Most respiratory infections are viral in nature, which do not respond to antibiotic therapy, so, unfortunately, your immune system must battle alone.
Pulmonary embolism
Pulmonary embolism occurs after a blood clot somewhere else in the body (often the legs) travels in the blood vessels to reach the lungs (via American Academy of Family Physicians). Risk factors for pulmonary embolism include recent surgery, increased estrogen exposure (such as hormone replacement therapy), recent travel, cancer, and others, according to Medical News Today.
These blood clots form as a result of three factors being present in varying concentrations. First, our venous blood flow must be moving slowly. This explains why our legs are a common location for a blood clot to begin. The veins in our legs use the muscle contractions of walking as a pump to send blood upwards to the heart. If we are not moving our legs, then blood may pool in the veins. The second important factor regards the health of the blood vessels themselves. If our blood vessels are narrowed due to cholesterol plaques, then blood will have to slow down to traverse the narrow vessels. It is akin to turning a three-lane highway into a one-lane road during rush hour — there will be traffic. Thirdly, changes to blood itself can increase the risk of developing a blood clot. Commonly, this is due to medications or organ dysfunction which make the blood somewhat thicker.
People with pulmonary embolism often describe symptoms of shortness of breath and chest pain that is worse with deep breathing. This is known as pleuritic chest pain. Pulmonary embolism is typically treated with an extended course of blood thinners prescribed by a medical professional.
Collapsed lung
Pneumothorax is more commonly known as a collapsed lung. The lungs sit in an airtight compartment in the ribcage. The pressure in this compartment must be lower than the pressure of the air so the lungs can expand. If there is a sudden increase of pressure in the ribcage, then the lung must overcome a greater force in order to expand with each breath. A collapsed lung, or pneumothorax, occurs when this pressure is far too high, making it impossible for the lung to expand (via Merck Manuals). In fact, on a chest X-ray, you can see the lung balled up within the ribcage.
This can cause chest pain that is more pronounced on one side of the chest. Further, breath sounds will be reduced on the affected side. Most cases of pneumothorax follow an injury to the lung itself, or a penetrating injury to the chest wall (gunshot wound, stabbing, or rib fracture). However, pneumothorax is a common complication from surgical operations that take place within the chest.
Pneumothorax is commonly diagnosed with chest X-rays, though other imaging modalities can also be helpful. To treat a pneumothorax, a medical professional must decompress the chest cavity and restore negative pressure. This is usually accomplished surgically with the placement of a chest tube. In this surgery, an incision is made in the muscles between the ribs and a tube is passed into the chest cavity (via Mayo Clinic). This tube is often connected to suction in order to restore the negative pressure our lungs need in order to breathe effectively.
Angina
"Angina pectoris, or angina for short, is the term used when chest discomfort is thought to be attributable to myocardial ischemia," Dr. Simon Mahler, professor of emergency medicine, explained in an article for UpToDate. Myocardial ischemia is the complicated name given to a decrease in oxygen in parts of the heart muscle. Dr. Mahler explained, "Myocardial ischemia is one of the more common causes of chest pain (also termed 'chest discomfort') in adults."
Typically, the pain of angina is described as a heaviness or pressure in the center of the chest. This type of pain is very similar to the pain caused by heart attacks. However, angina symptoms will get better within 20 minutes, according to Dr. Mahler. If you experience angina-like chest pain that is not improving with rest and time, it is imperative to be evaluated at the emergency department.
Angina itself is not dangerous, but it does direct a clinician to evaluate your risk factors for heart disease. So, if you experience angina, consider paying a visit to your primary care physician or a cardiologist.
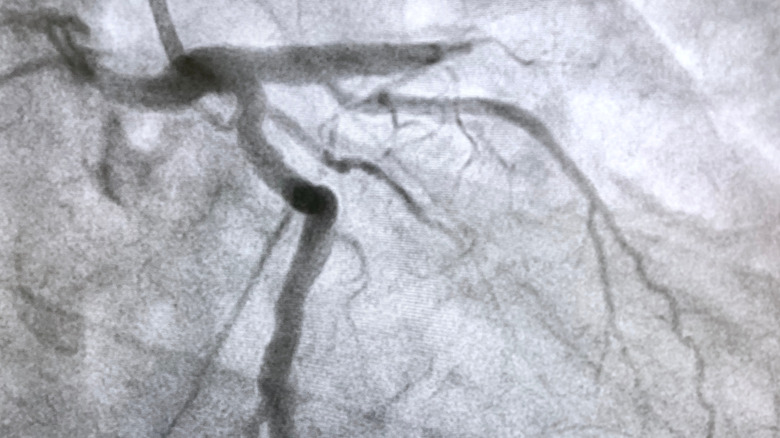
Acute coronary syndrome
Of course, when chest pain is felt, the first thing you may think of is heart attack — and that may very well be the cause. Heart attacks happen when a portion of heart muscle fails to receive adequate blood flow. Medical professionals broadly classify this as acute coronary syndrome, or, ACS (via Mayo Clinic). This can lead to tissue death that impacts the ability of the heart to do its job, leading to cardiac arrest and death of the patient. ACS can be broken down into myocardial infarctions (heart attacks) and a condition called unstable angina.
There are two types of myocardial infarction which, in general, are classified by how the present on electrocardiogram. These are ST elevated myocardial infarction (STEMI) and non-ST elevated myocardial infarction (NSTEMI), according to Merck Manuals. Both of these are very serious conditions. Unstable angina is a cousin of STEMI and NSTEMI and refers to chest pain that is neither relieved with rest nor a commonly prescribed drug called nitroglycerine. Unstable angina increases the risk of developing STEMI or NSTEMI and therefore should be investigated immediately.
Classically, the pain from ACS is described as an extreme pressure on the center of the chest, sometimes radiating to the arms. Sweating, clammy skin, and an impending sense of doom have also been described. However, not everyone with ACS experiences these symptoms. Women are more likely to describe atypical symptoms such as nausea or dizziness along with a general discomfort in the chest. ACS requires immediate treatment in the hospital in order to decrease the risk of death.
Pericarditis
The heart looks quite different from what Valentine's Day cards would have us believe. In actuality, the heart is tucked within a dual-layer sac of fibrous connective tissue called the pericardium. Between these layers is a thin amount of lubricating fluid allowing the heart to wiggle and pump within. However, the pericardium can become inflamed by a variety of factors. And, because of its close relationship to the heart, this can cause chest pain that mimics symptoms of a heart attack. When this occurs, it is called pericarditis.
According to the American Heart Association, "Pericarditis can be attributed to several factors, including viral, bacterial, fungal and other infections." When this condition develops quickly, it is called acute pericarditis. However, pericarditis can also develop over a longer period of time, called chronic pericarditis. Both types can result in compression of the heart, which can be dangerous. "In rare cases, pericarditis can have very serious consequences, possibly leading to abnormal heart rhythm and death," the American Heart Association warns.
Commonly, pericarditis is caused by a transient viral infection that will clear up on its own. However, certain autoimmune and chronic inflammatory conditions can result in an inflammation of the pericardium. Treatment is usually aimed at controlling symptoms of chest pain and inflammation, including non-steroidal anti-inflammatory medications like ibuprofen.
Congestive heart failure
Heart failure is a very frightening term. While chronic, congestive heart failure is a treatable disease (via Medical News Today). An article published in StatPearls noted, "Common etiologies of this type of congestive heart failure include severe anemia, thyrotoxicosis, obesity, nutritional deficiencies (thiamine deficiency, etc.), and pregnancy." This commonly occurs when the body is overfilled with liquids. The increased blood volume causes increased pressure in our blood vessels. This forces the heart to work harder than usual and can lead to failure of the pump.
Congestive heart failure often causes patients to complain of difficulty catching their breath and chest tightness or discomfort related to exertion. Classically, too, patients in congestive heart failure will have pitting edema. Congestive heart failure is definitively diagnosed through a procedure called an echocardiogram, per StatPearls. This is an ultrasound that measures how effectively the heart is working. Congestive heart failure is treated with oral medications, including diuretics and common blood pressure medications like ACE inhibitors.
Pancreatitis
Pancreatitis is the name given to inflammation of a spongy organ called the pancreas, which sits just below the diaphragm and between the stomach and the spine . Pancreatitis occurs when the tissue of the pancreas becomes inflamed, causing the leak of digestive enzymes. "In the majority of cases, alcohol use, gallstones, and hypertriglyceridemia cause acute pancreatitis," according to an article in StatPearls. Additionally, the article continued, "The patient will commonly describe moderate to severe abdominal pain located in the epigastrium with nausea and anorexia."
Because the epigastrium (space between the belly button and the ribcage) is in close proximity to the chest, the nervous system may confuse the location of the pain. For the pancreas, this often means radiating pain to the back and sometimes to the chest. This pain may be severe.
Thankfully, diagnosis and treatment of pancreatitis is generally straightforward. Diagnosis relies on a blood test that detects the enzymes amylase and lipase, which are produced by the pancreas (via Healthline). Treatment generally consists of supportive care, including IV fluids and pain medications.
Shingles
While we remain immune to chickenpox after inoculation, the virus never really goes away. Not to worry, for many people the virus remains at bay for our lives — it is simply kept dormant in the body. However, in older age and in times of acute stress, the virus can reappear as a disease commonly called shingles (via Johns Hopkins Medicine).
"[Shingles] is characterized by a painful, unilateral vesicular eruption, which usually occurs in a restricted dermatomal distribution," according to UpToDate. That means both pain and skin lesions will follow a bandlike strip of skin and will not cross the midline of the body.
Because shingles can appear on any patch of skin, the chest may be affected. As such, early shingles is a commonly missed cause of chest pain (via NJ Cardiovascular Institute). There is good news though, according to UpToDate, "Fewer than 20 percent of patients who develop a rash have significant systemic symptoms, such as headache, fever, malaise, or fatigue." Treatment of shingles may be accomplished with antiviral medications and pain management.