Winter Allergies: Everything You Need To Know
Itchy, watery eyes and runny noses brought on by seasonal allergies aren't just limited to the springtime. When nature gets frisky and the pollen count soars, many people have to reach for antihistamines — up to 60 million people annually in the United States, according to the Centers for Disease Control and Prevention. But as the days get shorter and temperatures drop, some folks can experience similar or intensifying allergy symptoms, and even asthma or eczema flares. What gives?
It turns out, more time at home — especially in winter when we close our windows and our homes get less ventilation — can increase our exposure to non-pollen allergens, with the main culprits being dust mites, pet dander, mold spores, and cockroaches. Ick!
Health Digest spoke with allergy experts to get the information you need to identify indoor allergens, reduce their presence in your home, and improve the snotty symptoms of winter allergies.
Symptoms of indoor winter allergies
When you have an allergy — whether in winter or any other season — your immune system identifies the allergen (whatever is causing the reaction, like pollen) as an infectious invader. Touching or breathing in an allergen causes an overactive defensive chain reaction in your body, releasing antibodies and later histamine, an inflammatory chemical that usually helps the body fight infection, but also causes unpleasant symptoms (via MedlinePlus).
Many traditional allergy symptoms fall under the category of allergic rhinitis, or inflammation of the nose, according to Dr. Janna Tuck, a New Mexico-based allergist and spokesperson for the American College of Allergy, Asthma, and Immunology. "Congestion, stuffy nose, sneezing, and itchy nose. Mucus production — a lot of snot — which can be from the front or down the back of the throat, which then can cause a cough or throat clearing" are all typical allergy symptoms, Tuck told Health Digest. Your eyes, ears, and even the roof of your mouth can also get itchy from allergies, Tuck said, and they can worsen asthma and eczema symptoms as well. Severe or chronic allergy symptoms can lead to fatigue and brain fog, Tuck added.
Is it winter allergies, cold, flu, or COVID-19?
Some indoor allergy symptoms, like runny nose and congestion, can overlap with those of viral respiratory infections, including the common cold, the flu, and COVID-19, according to the American Academy of Allergy, Asthma, and Immunology. But your body can give you clues about what's really happening.
Allergies don't cause fevers, for one thing, according to allergist Janna Tuck, and they don't usually cause sudden, severe body aches or fatigue. Instead, allergy symptoms ramp up gradually. "Usually you'll have symptoms for a week or two before you really start feeling terribly rundown with allergies, versus influenza in particular, you know, you'll feel fine and 24 hours later, you'll feel like a Mack truck hit you," Tuck told Health Digest.
Never noticed indoor allergies before? While it is possible to develop allergies at any point in life, it's more likely that your exposure level to an unknown allergen is what actually changed. Many of us used to spend significant time outside of our homes. Now that we're home almost 24/7, we're potentially being exposed to higher levels of allergens that were less plentiful at the office. That's especially true if you've welcomed a new pet into your life since the start of the pandemic.
How to identify indoor allergens
Once you begin noticing allergy symptoms, it's a good idea to start a little health diary (via WebMD). Where were you when your symptoms started? Maybe symptoms get worse when you visit certain pet-owning friends or relatives. Was anything different about that day? Perhaps your daily routine has changed significantly. Dated notes can also help you to notice patterns over time. Maybe symptoms crop up around the same time each year, like in the winter months.
Consider what's going on in your own home, too. Water damage, like from a flooded basement, leaky pipes, or poor window insulation can promote mold growth that can cause allergies. And new pets, even small ones like birds, rabbits, and hamsters, can turn out to aggravate allergies.
If you haven't been keeping notes, though, don't worry. Doctors are trained to help you figure it out. "Allergists have a tendency to take a pretty wide history to try to figure out what makes sense with a patient's symptoms," said Dr. Janna Tuck, an allergy specialist in private practice in Santa Fe, New Mexico.
Indoor allergen: dust mites
While dust bunnies may sound cute and seem harmless, allergy-inducing, invisible dust mites living large inside them are not. They're actually teeny-tiny relatives of spiders, with eight legs and a taste for dead skin cells, according to the American College of Allergy, Asthma, and Immunology (ACAAI). And they're all over your home.
"Dust mites are microscopic creatures that are present in our bedding, carpeting, upholstered furniture, heavy drapes, and even stuffed animals," said Payal Patel, an assistant professor and physician at Rush University Medical Center within the division of allergy and immunology. Dust mites thrive in warm places with high humidity, Patel told Health Digest, and allergists often see more patients with dust mite allergies in winter because people are spending more time indoors.
The ACAAI says dust mites also float around and can get puffed into their air like baby powder whenever fabric-like surfaces get disturbed, for example by vacuuming, walking on carpet, and rustling your bedsheets. Your home doesn't have to be visibly dirty or dusty to be overrun with dust mites, and overenthusiastic cleaning can sometimes just stir them up and make allergy symptoms worse.
Try these tricks to reduce dust allergy symptoms
How can you limit exposure to dust mites, which are invisible to the naked eye and love fabric? "One of the biggest things you can do in mitigating dust mite exposure is to get dust mite covers or encasings" to go underneath your bed sheets, said Payal Patel, a Chicago-based allergist. The best ones have zippers, she advised.
"You want to put that on your mattress, your pillows, even the boxspring," Patel said. Covers prevent the dust mites from settling into fabric surfaces that can't easily be washed. Then you should launder your bed linens in the hottest water possible once a week, Patel told Health Digest, to remove the dust mites.
Carpets should be vacuumed once a week, and maybe even upholstered furniture like your couch, Patel said, but it's important to use a vacuum with a HEPA filter, which will actually capture microscopic, allergy-inducing particulate matter like dust mites, instead of blowing it back into the air and aggravating allergies.
Indoor allergen: pet dander
We'll tell you the bad news upfront: There's no such thing as a hypoallergenic pet. When it comes to pets and allergies, "they have triggers that are located in their dander" — actually their skin, not their fur — "in their saliva, and in their urine, which is why there really isn't an allergy-free animal per se," according to Chicago-based allergist Payal Patel. When people with pet allergies inhale these proteins, they can experience symptoms like congestion or runny nose. If you're allergic to dogs, for example, and pet a pup and then touch your face, you could experience itchy or watery eyes.
But there is also good news! An allergist isn't going to make you get rid of your beloved four-legged floof. While some families may be willing to find new homes for allergy-triggering animals, "it's not for everyone, and an allergist understands that," Patel told Health Digest. You don't even have to keep your pet outside, which can be impractical advice for many folks due to extreme winter and summer conditions or individual living situations.
Pet-free zones and regular baths for Fido can provide respite from pet dander
If your fur baby is the culprit behind your winter allergy symptoms, don't despair. There are several steps you can take to decrease the pet allergen load in your home and come to a dander detente.
Establishing a pet-free zone or pet-free room can give allergy-prone folks a safe space from triggers. "That gives you a little reprieve where you can go and there's very limited dander and animal allergen exposure," Payal Patel, an allergy specialist and assistant professor at Rush University Medical Center in Chicago, told Health Digest. Strongly consider choosing your bedroom, so you can avoid resting your face on allergen-covered sheets.
An air purifier with a HEPA filter (it stands for high-efficiency particulate air) can also decrease the amount of invisible allergens floating around in high pet-traffic rooms; just be sure to get a purifier appropriate for the square footage of the space, Patel said. And don't forget to change filters per the manufacturer's frequency suggestions for optimal air. Bathing your pets weekly or every other week can also decrease the amount of allergens they're shedding, Patel added, but it's best done outside the home or at least by a non-allergy-having family member.
Indoor allergen: mold spores
Mold exposure is more of an outdoor allergen problem than an indoor one, even if your home has a musty-smelling quality to it. "The amount of mold [in the air] as soon as you walk out your front door is many, many times what the air is in your home," according to New Mexico-based allergist Janna Tuck. As a general rule, she told Health Digest, mold won't be pervasive in a house, but rather occurs in concentrated areas, and that's where people with mold allergies can get into trouble.
"If you're concerned about mold in your home, you need to look at your structure. You need to make sure you don't have leaks," Tuck explained. Our homes are made out of organic materials like wood, she said, so if water gets in, mold will grow. Things like poor insulation around windows and inadequate ventilation in bathrooms are just a few examples of mold waiting to happen.
If you do discover water damage in your home, Tuck said you're not doomed to have a moldy house forever. But you do have to be certain to find and correct the source. "You can rip out the drywall but if the roof is still leaking, it's going to get wet again," she said.
Identify mold and reduce your allergy symptoms
An inexpensive instrument called a hygrometer can measure humidity in the air and clue you in to possible mold hotspots. "You can sit those in a place for a while and go, 'Yep, that really is damp all the time.' Or, 'It's only damp when I take a shower,'" said allergist Janna Tuck. When you know for certain an area of your home has a humidity problem, you can start to game plan solutions.
If you're running the central heating a lot during the winter, consider keeping the fan on all the time. This can help move air and moisture more evenly throughout the house, Tuck explained. If you're still finding damp spots, consider calling heating and cooling specialists, who will be able to recommend appropriate mold-mitigating solutions.
If it's the bathroom giving you humidity problems and you don't have a built-in fan, keep the door open after showering to help humidity dissipate more quickly, and clean the shower and shower curtain regularly to keep mildew in check, Tuck advised. If it stays stuffy after showers, leaving a small fan in the doorway can help move air along.
Indoor winter allergen: cockroaches
As if these apocalypse-resistant pests weren't gross enough, cockroaches can trigger allergy symptoms for some people — about 20 to 40 percent of American adults and children, according to some studies. They're also in way more of our homes than we'd like to admit. According to a pest control trade group, cockroach allergens are present in over 60 percent of homes in the United States, and those rates are even higher in big cities (via the American College of Allergy, Asthma, and Immunology).
In the winter, these creepy crawlies make their way inside your home to get out of the cold and find food, according to Any Pest. The microscopic shedding body parts, saliva, and excrement of cockroaches all contain proteins that can aggravate both allergies and asthma when they're kicked up into the air, especially in children (via Healthline).
Asthma is the most common chronic illness in children. And according to a 2016 report in Allergy, 60 to 80 percent of kids living in urban areas who have asthma are allergic to cockroaches. So if you or your child has asthma, it's seriously important to get pests under control.
This is how you can keep the roaches at bay
To get nuisance cockroaches out of your home, it's helpful to make your home unattractive to them. The Asthma and Allergy Foundation of America has several useful tips: Use a trash can with a securely closing lid and store all food in airtight containers (we're looking at you, crumpled bag of sugar). Check under all the sinks in your home for leaking pipes, since cockroaches prefer humid climates. Sweep floors and clean off counters regularly to eliminate crumbs. Don't leave pet food out all day, and regularly wash your pet's food bowl.
Search your home for cracks in walls, around pipes, and in the floor where roaches could be getting in, and seal them off with caulk or joint compound from the hardware store. The Foundation recommends bait and traps instead of aerosol sprays, which can aggravate your symptoms even more, but use caution since some products may be toxic for pets or children. If all else fails, find an exterminator. These pros will have stronger tools in their bug elimination arsenal and the expertise to use them.
When to call your doctor about your winter allergy symptoms
Luckily for folks with allergies, there are more over-the-counter allergy medicines today than 20 years ago, and they have fewer side effects. But if you've been having symptoms consistent with allergies and you can't figure out what's triggering them, or over-the-counter remedies aren't giving you relief, call your doctor.
"It's never bad to speak with your primary care provider to start with," said Janna Tuck, an allergy specialist and a spokesperson for the American College of Allergy, Asthma, and Immunology. Your primary doctor knows your history, and can discuss other potential causes for your symptoms. But if you have a family history of allergies or asthma and you're having a hard time getting symptoms under control, it's probably fine to seek out an allergist directly, Tuck told Health Digest.
Before your appointment, Tuck advised, it's a good idea to write out your symptoms, what you think may be triggering them, any medicines you've tried, and what you hope to get out of your visit, all of which can streamline the process. When you schedule your appointment, you may also be told not to take antihistamines for a certain number of days beforehand, to ensure more accurate test results.
What does an allergy test entail?
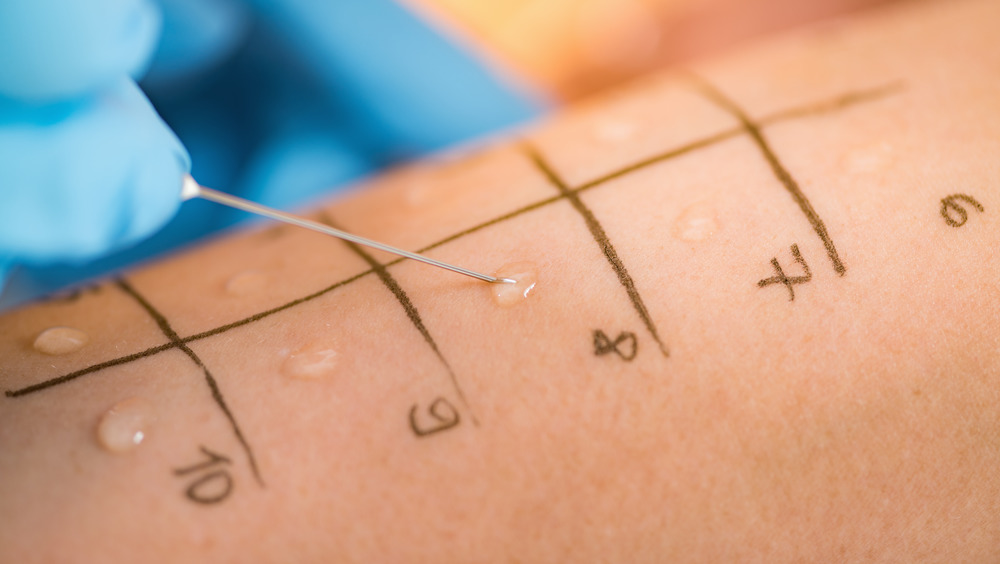
If you and your allergist are unsure what's causing your winter allergies, they can usually perform a same-day allergy test. The process involves pricking the skin on your back (but don't worry, you won't bleed) with small amounts of different potential allergens. It could be one prick or 50, depending on your symptoms. "But in general, if you're going for a snotty nose, we're probably going to do a large panel of things that are important for the area of the country you live in," said Dr. Janna Tuck, an allergy specialist in private practice in Santa Fe, New Mexico.
The doctor will wait for 15 to 20 minutes to see if your skin has an allergic reaction to any of the pricks, usually manifesting as an itchy red bump, Tuck told Health Digest. And if you do get super itchy or bothered, your allergist can give you a topical or oral medicine to calm the reaction, which should subside by the end of the day.
Treatment options for indoor allergies
Once you discover the cause of your winter allergy symptoms, your doctor will work with you to develop a treatment plan, involving environmental changes, medicine, or both. Medications include pills, nasal sprays, and eye drops that can help block the bothersome effects of histamine. Other medicines may help reduce inflammation associated with allergies. Dr. Payal Patel, an allergist at Rush University Medical Center in Chicago, says these medicines are a good starting point for managing symptoms, but they won't actually change the way your body responds to allergens. "But it will improve your quality of life, reduce your symptoms, and help you feel better," she told Health Digest.
What can change the way your body responds, Patel said, is desensitization or exposure therapy, aka allergy shots. Although the process can take three to five years, regular allergy shots slowly expose your body to the things you're allergic to, and eventually can change your immune response so you can stop or decrease the amount of medicine you need to control your symptoms.
"The allergist will go through all the different options you have at your disposal and all the pros and cons of each, and then a patient can make that decision as to what fits their lifestyle the best," Patel said.