Bacterial Vaginosis Explained: Causes, Symptoms, And Treatments
The vagina normally houses different types of bacteria, maintaining a type of balance within it (via Cleveland Clinic). Bacterial vaginosis occurs when this balance is disrupted and certain bacteria grow in number. This leads to an infection, with a few noticeable signs.
Bacterial vaginosis is pretty common. It affects about 21 million American women aged 14 to 49 years, a period between puberty and menopause (via the Centers for Disease Control and Prevention). Bacterial vaginosis is also the most common reason why women in this period produce an abnormal vaginal discharge, notes the Cleveland Clinic.
The symptoms experienced by women with bacterial vaginosis can be a source of embarrassment or self-consciousness. Affected women may also avoid doing regular things like having sex, going out with someone new, or exercising. Bacterial vaginosis might not get properly treated because many women mistake it for a yeast infection (thrush) or might not be aware of the risks of the condition (per the American Sexual Health Association). Fortunately, this condition can be detected and treated. Early treatment is necessary, because bacterial vaginosis can lead to other serious illnesses If left untreated (via WebMD).
Bacteria that live in the vagina
The thought of bacteria living in your vagina might be horrifying, but the reality is that there are good bacteria all over your body. You may have even heard that these microbes live in your gut or on your skin.
About 10 billion bacteria also live in your vagina and form the vaginal microbiome, according to a 2021 review in Frontiers in Cellular and Infection Microbiology. Each woman has a unique vaginal microbiome due to differences in race, sexual activity, stress levels, and socioeconomic situations. In one person, the vaginal microbiome might be modified by douching, getting older, hormonal changes (such as during pregnancy), immune responses, the use of antibiotics, exposure to harmful microbes, or infections.
Per a 2021 review in Antibiotics, the lactobacilli are the most numerous bacteria species in the vagina of most women. And the lactobacilli don't live rent free: They keep harmful bacteria at bay by making your vagina acidic, producing antimicrobial substances to kill them, influencing your immune system, and occupying your vagina so thoroughly that the harmful bacteria won't have resources to live on. The lactobacilli maintain the balance within the vaginal microbiome. But there's always a struggle between the lactobacilli and other harmful bacteria to occupy your vagina, states News Medical. Bacterial vaginosis happens when the lactobacilli lose their dominance and harmful bacteria increase in number.
How to know if you have bacterial vaginosis
Abnormal symptoms within your vagina area will let you know that something is wrong. But many women with bacterial vaginosis (about 84%) have no symptoms, per the CDC.
For some women, the symptoms are so mild that they don't see that something is wrong. Most women who show symptoms experience an increased volume of watery vaginal discharge (via Planned Parenthood). This discharge could come in different colors (white, gray, or green) and may have a foamy consistency. The discharge may also have a foul fishy smell that gets worse after vaginal sex. Other less common symptoms are an itchy vagina area and a burning sensation that comes with peeing. It's normal for your vagina to produce transparent or whitish discharges of different consistencies and volumes throughout the month (per Cleveland Clinic). This is usually different for every woman. But your discharge shouldn't come in a strange color, have a bad smell, foam, or suddenly be produced more than what you've noticed before.
Bacterial vaginosis and a yeast infection share similar symptoms. Unlike a yeast infection, the discharge of bacterial vaginosis is watery and has a fishy smell. The vulva (the outer part of the female genitals) doesn't get inflamed or red like it does with a yeast infection (per Medical News Today). Unusual symptoms from your vagina can point to a number of conditions. WebMD advises that you visit your doctor if you notice a smelly discharge that comes with a fever.
How is bacterial vaginosis diagnosed?
The best way to confirm that you have bacterial vaginosis is to get tested. Your doctor will want to know about your symptoms and if you've had any previous sexual health issues like sexually transmitted infection (STIs) or other vaginal infections (via Mayo Clinic). They may use a pH test strip to check the acidity of your vagina. A pH level above 4.5 might indicate that you have bacterial vaginosis. Samples of your vaginal discharge will be taken for a lab test to check its bacterial composition and confirm whether you have bacterial vaginosis.
To get good results, doctors recommend that you don't set an appointment while you're menstruating. You should make sure that you don't have sex or douche the day before your appointment (via the National Institute of Child Health and Human Development). It's also important that you don't insert anything into your vagina (like a tampon or sex toy) or irritate your vagina with things like vaginal sprays before your appointment.
Familydoctor.org suggests that you talk to your doctor about your test results, the probable cause of your condition, and treatment options available to you. You can also ask how long bacterial vaginosis will last and whether it's safe for you to have sex during the period.
How do you get bacterial vaginosis?
You get bacterial vaginosis when the balance of your vaginal microbiome is disrupted, a fact that has been known for over 100 years (per a 2017 review in Obstetrics and Gynecology. But what actually disrupts the vaginal microbiome has not been fully outlined.
So far, certain factors that increase a woman's chance of getting bacterial vaginosis have been identified. These include douching, smoking, obesity, and a diet that doesn't have a variety of nutrients or contains too much fat or sugar. The National Women's Health Network adds that using any product containing fragrances or irritants on your vagina, as well as wearing non-breathable clothes too often, increases your risk of getting bacterial vaginosis.
An imbalance within the vagina microbiome means that the lactobacilli are less than they should be. Consequently, the vagina loses its acidity and ability to ward off harmful bacteria. This encourages the growth of harmful bacteria like Gardnerella, as the environment within the vagina becomes more hospitable towards them (via Access Medicine). The overgrowth of these harmful bacteria produces the discharge noticed by women with this condition. Also, the harmful bacteria produce substances rich in amines that give off a fishy smell.
Can you get bacterial vaginosis through sex?
Bacterial vaginosis and sex have a complicated relationship. Even though what tips the balance of the vagina is not completely understood, it's also not proven that this is caused by harmful bacteria passed during sex. A woman could get bacterial vaginosis without having sex even though most women who get it are sexually active. Moreover, treatment of male sex partners of women with this condition doesn't help them get rid of it. So, bacterial vaginosis is not regarded as a sexually transmitted infection, per the CDC's guidelines.
There are several risk factors for bacterial vaginosis outside sex but sex plays an important role. For instance, the majority of women in a study published in PLOS One recognized their symptoms after a sex encounter. This included sex with a regular partner or a new one. Like other STIs, having sex for the first time at a young age, not using protection, having multiple sex partners, or recently getting a new partner increases your risk of getting bacterial vaginosis (via a review in BMC Medicine). Lastly, a review published in PLOS One adds that having sex with a female partner who has bacterial vaginosis increases your risk of getting it.
How you can prevent bacterial vaginosis
Patient.info notes that since the cause of bacterial vaginosis cannot be traced for many women, trying to prevent it might be difficult. However, avoiding practices known to mess with the balance of your vaginas bacteria may be helpful. These include douching, the use of scented hygiene products, washing your vagina many times in a day, using harsh detergents to wash your panties, and wearing tight clothes. The site also advises you to take showers instead of baths, and to avoid taking baths with antiseptics, bath oils, and perfumed products. When you have sex, use a water-based lubricant, and always use a condom. The Office on Women's Health advises using condoms to cover sex toys and a dental dam for oral sex with a female partner. They also advise that you don't keep multiple sexual partners or avoid sex totally.
A good diet can help you prevent bacterial vaginosis, according to a review published in Polish Gynecology. Fruits, vegetables, milk, dairy products, legumes, and seeds reduce your risk of getting bacterial vaginosis because they contain essentials like calcium, vitamins A, C, D, E, folic acid, and beta carotene. There are also some foods items you should avoid. Sweets and other sugary foods can weaken barriers against harmful bacteria by causing oxidative stress and weakening your immune system. Also, a diet high in fat makes your vagina less acidic and weakens your immune response.
Bacterial vaginosis has negative effects on women's health
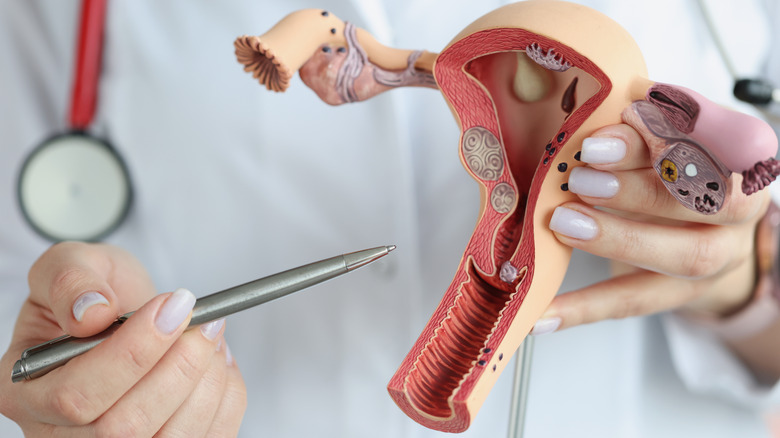
Bacterial vaginosis has many detrimental effects to health if left untreated. The harmful bacteria that invade the vagina do not remain there, but spread and infect surrounding parts of the female genital tract, according to a review published in Frontiers in Cellular and Infection Microbiology. This can lead to urinary tract infections and inflammation of the cervix, walls of the womb, and the fallopian tubes. Once these bacteria invade and infect the womb or fallopian tubes, they can cause an illness known as pelvic inflammatory disease. Women can also get cervical cancer or tubal infertility (blockage of the fallopian tubes) from bacterial vaginosis. It also increases the risk of getting infections after surgical procedures like a hysterectomy, the surgical removal of the womb.
Bacterial vaginosis makes it more likely that you'll get an STI especially if you are vulnerable, per a review published in Military Medical Research. Women who have bacterial vaginosis have a 60% increased risk of getting human immunodeficiency virus (HIV). This may be because a less acidic vagina encourages the survival of the virus. Bacterial vaginosis also increases your chances of getting herpes, syphilis, gonorrhea, and chlamydia. Thus, women with bacterial vaginosis must use protection, avoid sex with multiple people, and avoid sex with anyone who has an STI.
Bacterial vaginosis is associated with infertility and negative pregnancy outcomes
In addition to its effects on genital health, having bacterial vaginosis during pregnancy can cause complications. According to a review published in Frontiers in Public Health, bacterial vaginosis is associated with spontaneous miscarriages, preterm premature rupture of membranes (when your water breaks before the 37th week of pregnancy), preterm labor, and preterm birth. Bacterial vaginosis is also associated with infection of the placenta and amniotic fluid, infection of the genital tract during or after labor known as puerperal sepsis, and infections of the wound from a cesarean delivery. Why these complications happen as a result of bacterial vaginosis is not fully understood, but they likely result from the harmful bacteria that travel up the genital tract.
For women who wish to get pregnant, bacterial vaginosis likely increases the risk of infertility, notes a review published in the American Journal of Obstetrics and Gynecology. It is still not perfectly clear how bacterial vaginosis causes infertility. It could be because of the body's immune response to the harmful bacteria which may not favor fertility, or because these harmful bacteria are able to go up into the genital tract and block the fallopian tubes. The conditions associated with bacterial vaginosis are linked with infertility as well. Pelvic inflammatory disease and endometritis increase the risk of infertility. Bacterial vaginosis increases the risk of getting STIs, and these STIs increase the risk of infections of the upper genital tract, pelvic inflammatory disease, and infertility.
How is bacterial vaginosis treated?
Although bacterial vaginosis could go away on its own, it requires treatment with antibiotics in many cases (via Medical News Today). It is usually treated using metronidazole (Flagyl). This could be in the form of pills, single doses that come in one packet, or vaginal gels. If metronidazole doesn't work or can't be used, clindamycin (Cleocin) or tinidazole (Tindamax) may be used. Tinidazole is available in pill form, while clindamycin can be taken as pills, vaginal ovules, vaginal gels, or vaginal creams. You should avoid using products made from latex such as condoms, diaphragms, or cervical caps for protection when you use clindamycin ovules and creams, as they weaken latex and may render these products ineffective.
The CDC recommends that pregnant and non-pregnant women who have symptoms of bacterial vaginosis get treated. This treatment is needed so women can reduce their risk of getting STIs and other diseases, as well as avoid negative pregnancy outcomes. Additionally, women are encouraged to schedule a follow-up if their symptoms come back. Meanwhile, the treatment of male sex partners is not recommended, as it does not improve treatment for women with bacterial vaginosis.
Are probiotics good for bacterial vaginosis?
Probiotics are live microbes that have health benefits when taken in sufficient quantities (via a review published in Current Opinion in Pharmacology). Much like the vaginal lactobacilli, probiotics containing lactobacilli could benefit the vagina through different methods. They alleviate the immune reaction of the body to harmful bacteria by competing with and killing these invaders. Probiotics can also restore the vagina to its normal status after a bacterial vaginosis episode and prevent it from coming back.
There is some debate about the effectiveness of probiotics for the treatment of bacterial vaginosis, though. Researchers in a 2019 meta-analysis, published in the International Journal of Environmental Research and Public Health found that the use of probiotics alone or with antibiotics are beneficial for the treatment of bacterial vaginosis. Probiotics used alone showed long-term benefits, while probiotics used with antibiotics provide short-term benefits. Another 2022 meta analysis, published in Reproductive Health, found that probiotics are just as good as antibiotics for the treatment of bacterial vaginosis. Plus, probiotics used with antibiotics are more effective than antibiotics alone. While these meta analyses show that probiotics for the treatment of bacterial vaginosis can be effective, both note that better studies still need to be done on how to use probiotics.
Does bacterial vaginosis come back?
Treatment is usually effective in getting rid of bacterial vaginosis. Unfortunately, for many women, this is only short-lived.
Studies have shown that bacterial vaginosis comes back multiple times for many women, leading to a recurrent condition. This often happens within the year of the initial treatment (via a review in the European Journal of Obstetrics & Gynecology and Reproductive Biology). Recurrent bacterial vaginosis could be as a result of relapse of the previous infection or a reinfection. A relapse might happen if the condition isn't treated properly, or if the lactobacilli fail to dominate the vagina after treatment. Sexual partners of women with bacterial vaginosis can store the harmful bacteria and cause their reinfection post-treatment.
The same medications you took for your initial episode might be used if bacterial vaginosis comes back. Your doctor might increase the dose or duration of the treatment, or might decide to use a new medication. Your doctor might also prescribe boric acid inserts to get rid of the condition (via UpToDate). Although you can't tell if or why bacterial vaginosis will come back, it's best to complete the treatment of bacterial vaginosis to prevent a relapse. You can avoid getting reinfected by using protection while having sex. Healthline adds that you can reduce the risk of bacterial vaginosis coming back by practicing better hygiene (e.g., not douching, wiping from front to back), not using scented products, wearing breathable clothes, and reducing stress by exercising, yoga, or deep breathing.