Yeast Infections Explained: Causes, Symptoms, And Treatments
Have you ever experienced an uncomfortable itch or swelling in your vulva or vagina? If the answer is yes, then chances are you were having a yeast infection, also known as vulvovaginitis — a medical term that literally translates into inflammation of the vulva or vagina, according to the National Library of Medicine.
Yeast infections are very common, and they're primarily caused due to an infection with Candida fungus species (Candida albicans being the most common example). In such cases, the infection is referred to as vaginal candidiasis or candidal vulvovaginitis. However, a 2014 study published in Mycoses says that while Candida albicans is responsible for about 90% of yeast infections, they can also be caused by other Candida species such as Candida glabrata or Candida tropicalis. These infections are classed as resistant and opportunistic, meaning they are more likely to resist antibiotic treatment and affect people with weakened immune systems.
While yeast infections are not dangerous, they certainly are inconvenient, upsetting, and, in some cases, painful. Plus, they can also cause embarrassment, negatively impact sexual life, or become disabling due to the overall discomfort. Luckily, because they are so common, treatment is relatively quick and easy.
Yeast infections are caused by a fungus overgrowth
Candida albicans — the fungus responsible for most yeast infections — is a normal part of the vaginal flora, the microorganisms that normally live in the vagina, which include both yeasts and bacteria (per the Mayo Clinic). However, when the balance between healthy bacteria (such as Lactobacillus) and not-so-healthy microorganisms (such as Candida) is disturbed, an overgrowth of yeast occurs, resulting in a vaginal infection.
There are multiple factors or scenarios that disrupt the balance, making it easier for yeast to thrive and thus leading to yeast or fungus overgrowth. They include uncontrolled diabetes (in which high blood sugar levels "feed" the yeast), a weak immune system, antibiotic use (which kills both harmful and beneficial bacteria alike), and pregnancy or taking hormonal therapy such as oral contraceptives (which lead to an increase in estrogen levels).
In addition, a 2021 study published in the journal Diagnostics says that a change in your vagina's acidity or pH level is another determining factor for yeast infections. According to the study, the normal vaginal pH ranges from 3.8 to 5 — fairly acidic, which keeps harmful microorganisms at bay. When the amount of protective bacteria declines, the vaginal pH increases, allowing yeast to multiply and spread. Some common causes of variations in vaginal pH are unprotected sex, vaginal douching, menstrual cycle changes, and, again, antibiotic use.
Prevalence of yeast infections
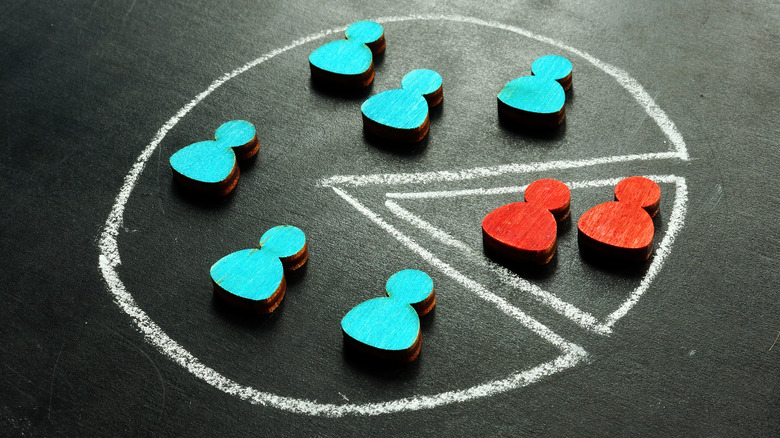
According to the Centers for Disease Control and Prevention, yeast infections are very common in people of reproductive age. In fact, it is estimated that about 75% of women worldwide have had vaginal candidiasis at some point in their life, and up to 45% of them have it multiple times in a single year. However, the National Library of Medicine explains that detailed data can be challenging to obtain because not all people with vaginal candidiasis seek professional treatment. This is due to two main reasons: the wide availability of over-the-counter drugs, and the fact that roughly 10% of the cases don't present any symptoms (meaning they don't even know they have it).
Given the high rates and frequency of yeast infections, the disease is also associated with high medical costs, representing a significant economic and public health burden. For instance, per a paper published in the journal Clinical Infectious Diseases, the total cost of candidiasis treatment for outpatients — those who received treatment without being admitted to a hospital — in the United States was almost $2.1 billion as of 2017, out of which $368 million were for vaginal candidiasis.
Symptoms of yeast infections
According to the Mayo Clinic, symptoms of yeast infections can vary from mild to moderate, and they commonly include redness and swelling of the vulva (the outer part of the vagina), itching in the vagina, vulva, or both, vaginal pain and inflammation, or vaginal rash. People with yeast infections may also experience a burning feeling during sex or when they pee. Furthermore, they might also notice changes in their vaginal discharge, which may range from watery to thick and white (often described as having a cottage cheese appearance).
Keep in mind that not all symptoms will appear at the same time. In some cases, people can show no signs at all, and those with infection due to Candida glabrata tend to show milder symptoms (per the National Library of Medicine). In addition, it is typical for symptoms to increase right before the menstrual cycle begins — a.k.a. when people get their period.
Lastly, the main difference between complicated and complicated infections' symptoms relies on their severity. In this case, people can develop extreme inflammation, redness, and itching, leading to sores or tears in the vagina or vulva (via the Mayo Clinic).
Classification of yeast infections
Depending on their frequency and how they respond to treatment, yeast infections can be classified as uncomplicated or complicated (per the Centers for Disease Control and Prevention). Furthermore, both types can be sub-classified into different categories depending on the characteristics of either the infection or the host.
For example, the CDC categorizes uncomplicated yeast infections into sporadic or infrequent, mild-to-moderate, likely to be Candida albicans, and those that happen to people who don't have a compromised immune system. In contrast, complicated infections are sub-classified as recurrent, severe, non-albicans candidiasis, and the ones present in people with underlying and compromising conditions. It is believed that about 20% of women present some type of complicated yeast infection.
Among complicated infections, recurrent infections are defined as having three or more episodes per year, affecting about 45% of women. As for severe infections, those are the ones linked to inadequate treatment response. Lastly, the most common compromising conditions that increase the chance of complicated infections are uncontrolled diabetes, immunosuppression therapy, HIV infection, and pregnancy.
Other types of yeast infections
Candida is also naturally present in other parts of the body, such as the mouth, digestive tract, and skin. Therefore, the vagina is not the only place where people can develop yeast infections. Yet, when an infection happens in other parts of the body, it is called thrush (according to the Cleveland Clinic). A Candida overgrowth also causes thrush, and while it can affect anyone, it is more common in newborns, toddlers, the elderly, and people with weakened immune systems. Because yeast thrives in moist or humid environments, thrush can be developed in the mouth and throat and the nipples or breasts of breastfeeding moms (per the Office on Women's Health).
The Cleveland Clinic explains that a thrush infection in the mouth or throat — also known as oropharyngeal candidiasis — is not a major health problem, and is usually not contagious in healthy people. Some of its most common symptoms include white wounds in the tongue and cheeks, redness and soreness, and loss of taste.
As for thrush during breastfeeding, it can be passed on from the baby to the mom or vice versa. For this reason, both mom and baby should be treated at the same time, even if only one of them presents symptoms. According to the Office on Women's Health, common symptoms of thrush during breastfeeding include sore, flaky, itchy, cracked, dark pink or blistered nipples; achy breast; or a shooting pain during or after feedings.
Men can also get yeast infections
While yeast infections are far more common in people assigned female at birth, they can also happen to people assigned male at birth. In this case, the infection is known as balanitis (per the Mayo Clinic).
Since Candida is usually present in the skin and thrives in humid environments, balanitis is characterized by an inflammation of the head of the penis. Therefore, uncircumcised people have a higher risk of developing it, as well as those with uncontrolled diabetes, excess weight, a weakened immune system, poor hygiene, and those who are under long-term antibiotic treatment. Also, having sex with someone with a vaginal yeast infection can increase the chance of Candida overgrowth and infection.
Lastly, much like vaginal candidiasis, balanitis can lead to itching and redness on the penis, a burning feeling while peeing or having sex, and accumulation of a thick and white substance in skin folds or areas of the penis with white skin.
Yeast infection diagnosis
Regardless of the site of infection, yeast infection diagnosis starts with a series of questions from your healthcare provider so that they can assess your overall health and become familiar with your medical history, including past infections — both sexually transmitted or caused by yeast overgrowth (via the Mayo Clinic).
In the case of vaginal candidiasis, the best way to diagnose it is through a pelvic exam, which generally includes an external evaluation to check for sores or other symptoms or abnormalities, followed by an internal exam in which your doctor checks the vagina and cervix using a speculum, a device that helps keep the vaginal walls open. Pelvic exams are relatively quick and don't require previous preparation, and while they can be a bit uncomfortable, they shouldn't cause any pain, the Mayo Clinic says.
Lastly, testing vaginal fluids might also be necessary. This will allow your doctor to determine the best course of action for the infection, which may require different treatments depending on the type of yeast responsible for the disease. Note that despite the growing popularity of at-home vaginal pH tests, people should always consult with a doctor if they suspect having a yeast infection, because these tests can only tell whether the vaginal pH is off or not — they cannot confirm an infection (via Healthline). Thus, self-diagnosing is never a good idea, even if you've had an infection before.
Risk factors
There are numerous factors that can increase the risk of developing a yeast infection, including lifestyle circumstances, certain medications, and health conditions. According to a 2021 study published in the Journal of Midwifery and Women's Health, some usual lifestyle factors for vaginal candidiasis include wearing tight or wet clothes, nylon underwear, or polyester pants because they promote a dark and moist environment that's perfect for yeast overgrowth. Additionally, per a 2021 study published in the journal Diagnostics, unprotected sex can also increase the risk of infection because semen has a pH of 8 — meaning that it is on the alkaline side, and thus can alter the vagina's acidity level.
Furthermore, the National Library of Medicine states that one risk factor for acute vaginal candidiasis associated with health conditions and medications is having high estrogen levels, which can result from external estrogen use from hormonal oral contraceptives or for endogenous or internal reasons (such as pregnancy or obesity). Moreover, people with health conditions such as diabetes, HIV infection, and chemotherapy or transplant patients have an increased risk of Candida overgrowth. In contrast, people with chronic or recurrent infections may have a genetic factor that makes them more susceptible.
Yeast infections: neither STD nor UTI
Yes, unprotected sex and having sex with a person with candidiasis or balanitis can increase the chance of infection. However, yeast infections are neither a sexually transmitted disease (STD) nor a urinary tract infection (UTI).
STDs can be caused by bacteria, viruses, or parasites, and they're transmitted by unprotected sex. Unlike yeast infections, they are severe conditions. Still, they have a couple of symptoms in common, including itching and a burning feeling around the genitals (according to the Cleveland Clinic). Nevertheless, per the Office on Women's Health, yeast infections are not considered an STD because you can also develop them even if you're not sexually active.
On the other hand, UTIs are caused by bacteria, and they can affect any part of the urinary system, such as the kidneys, bladder, ureters, or urethra. Therefore, while UTIs and yeast infections also share the burning-like symptom when peeing, they're two different infections. Like yeast infections, you can also get a UTI regardless of your sexual activity, and they can also be easily treated. However, note that antibiotics used to treat UTIs can lead to yeast infections (via Healthline).
Yeast infection treatment
Yeast infections are relatively easy to treat. However, treatment may vary depending on the type of yeast and whether you're dealing with a complicated infection or not.
For the most part, yeast infections can be treated with over-the-counter (OTC) antifungal drugs, meaning that you don't need a prescription (via Medical News Today). They are available in multiple forms, including creams, ointments, pills, or vaginal suppositories (a form of medicine that is inserted into the vagina, which is slowly dissolved and absorbed into the bloodstream).
The Office on Women's Health also explains that while certain treatments only require a single dose, others might need a daily application for up to a week. Nevertheless, recurrent or severe infections that keep coming back or don't go away after treatment with an OTC drug might need a different approach, such as taking weekly doses of antifungal medicine for up to six months. In addition, according to the Urology Health Foundation, changing the type of birth control might sometimes be a necessary part of treatment for complicated vaginal candidiasis. Lastly, circumcision may be needed in cases of balanitis that don't respond well to creams applied on the skin.
Considerations for yeast infection medicine
Once the proper medication for treating a yeast infection has been determined, there are a couple of important considerations you should keep in mind to ensure it works as effectively as possible. For starters, per a study published in the Journal of Midwifery and Women's Health, it is crucial to use the medication completely according to medical instructions even if the symptoms have already disappeared to keep the infection from returning.
Furthermore, the study provides a couple of tips for using vaginal suppositories. First, avoid applying them with dirty hands. You should always wash your hands before and after inserting the medicine. Second, given that the suppository is meant to be inserted high into the vagina, you might want to try it while lying down instead of doing so in an upright position. Third, use vaginal suppositories before going to bed to give the medicine plenty of time to do its job while you sleep and reduce leaking.
The study also indicates that it is normal to feel a slight irritation the first time you use a vaginal suppository — although be sure to talk to your healthcare provider if the discomfort persists. And last but not least, the study warns that some suppositories may cause damage to latex contraceptives such as condoms or diaphragms, which could increase the chances of pregnancy or STD. Therefore, you might want to wait till the end of your treatment to avoid any unwanted side effects.
Tips for preventing yeast infections
Given that some risk factors for yeast infections are linked to lifestyle choices, that means some of them can be easily modified to help prevent future infections. For example, the Cleveland Clinic suggests avoiding douching to keep from killing the vagina's protective bacteria, as well as refraining from using scented feminine products (such as tampons, pads, or feminine deodorants), which can alter the vagina's pH levels. Additionally, the site recommends changing out of wet clothes as quickly as possible — this includes bathing suits, gym clothes, and even sweaty underwear during a hot summer day.
What's more, per the Ontario Ministry of Health, another way to prevent infections is by wiping from front to back when going to the bathroom — both when you pee or poop — as this helps keep the germs from the anus from spreading to the vagina. Lastly, consider choosing underwear made from breathable materials such as cotton instead of nylon, and opt for loose clothes over fitted ones to help keep the vagina dry and promote healing.
When it comes to non-modifiable health conditions, the Cleveland Clinic states that controlling the reason for the infection can improve future outcomes or prevent yeast infections in the long run. For example, in the case of diabetes, keeping blood sugar levels as controlled as possible is one way to prevent yeast overgrowth.
Probiotics may help prevent infections and improve treatment
Probiotics are healthy microorganisms that have been used for years to improve gut health — most likely because the gut houses about 100 trillion friendly bacteria (per Livestrong). However, since Candida overgrowth is linked to an imbalance of the vaginal flora, researchers have evaluated the potentially beneficial effects of using probiotics for vaginal infections (via Healthline).
According to a 2021 clinical trial published in the journal Current Medical Mycology, probiotics have the ability to maintain and recover an imbalanced vaginal microbiota, meaning they have the potential to prevent Candida overgrowth. The trial determined that probiotics could help prevent yeast infections by lowering or acidifying the vagina's pH, improving the vaginal defense barrier against yeasts, and improving vaginal flora. Furthermore, the study determined that supplementing antifungal treatment with probiotics significantly improved symptoms of vaginal candidiasis, including itching and burning.
Similarly, another study published in Letters in Applied Microbiology found the same results and determined that probiotics from Lactobacillus species can increase the effectiveness of antifungal drugs. However, both studies state that probiotic use for yeast infections is still controversial in the medical community. In fact, a 2015 review published in Nutrición Hospitalaria points out that while probiotics can prevent recurrent infections, it is unlikely that they can replace antibiotics (and that further research is still needed).
A high fat and added sugar intake might increase the risk of infection
Just as your clothes or hygiene products can increase the risk of yeast infections, what you eat can also influence Candida overgrowth. A 2020 review published in Polish Gynecology explains that a high sugar and fat intake are the two main ways your diet might sabotage vaginal health.
According to the review, consuming too many simple sugars promotes an imbalance in the vaginal flora, providing favorable conditions that make it easier for yeast to grow uncontrollably. In addition, the study warns that long-term, high-fat diets can affect the way your body defends itself from harmful microorganisms because of the detrimental effects of unhealthy fats on the immune system.
Likewise, another study published in The Journal of Nutrition found that the risk of infection in women with greater fat intake was twice as high as in those who consumed fewer fats. Furthermore, the researchers determined that unhealthy or saturated fats — which are predominantly found in fast foods and bakery products — were a predicting factor for vaginal infections, seeing that they have the ability to increase vaginal pH. Thus, both studies recommend following what's popularly known as a Candida diet, which focuses on reducing the intake of fast foods and sweets and increasing the intake of fruits, vegetables, and dairy products.