Things You Should Never Do After Having Surgery
Prior to the unique circumstances presented by the COVID-19 pandemic, the average surgical burden on an American hospital was around 17.2 million procedures per year, both inpatient and outpatient, per the federal government's Agency for Healthcare Research and Quality. And that's not even taking into account surgeries performed in doctors offices and by dental surgeons in their offices. Despite the fact that the pandemic initiated a dramatic drop in nonessential surgeries being performed in the U.S., once hospitals and medical staff got up to speed with the resulting increase in demand for acute healthcare services amid the pandemic, those numbers returned to normal, according to Stanford Medicine.
Moreover, the average American will, over the course of their lifetime, undergo at least seven surgical procedures, according to surgeon and Harvard Medical School professor Atul Gawande, per NPR. A 2008 scientific study in which Dr. Gawande was a lead author put that number even higher — at more than nine per lifetime, including at least three inpatient operations, two outpatient operations, and three non-invasive surgical procedures (per Journal of the American College of Surgeons).
In other words, in one way or another, surgery is coming for you at some point, even if it's just a minor, non-invasive procedure. Planning ahead is still one of the best ways you can ensure that your surgery will be a success, according to the American Society of Anesthesiologists. And planning includes knowing how your activities will be restricted in the days and weeks while your recover.
Never drive soon after undergoing general anesthesia
One thing you should never do after surgery is anything your doctor has told you not to do, according to Healthline. That might sound both obvious and reasonable now, but wait until you're sitting across from your doctor and they tell you that you shouldn't be driving. The fact is, any surgery that involves general anesthesia will be followed by that instruction. The reason is that even after you emerge to wakefulness, you are still under the influence of the drugs that put you under until the have time to fully leave your system. For as long as you are still under the influence of these drugs, it is presumed that you will be impaired, both neurologically and cognitively, even if you think you're perfectly fine.
Neurologically speaking, anesthesia slows reflexes, per Verywell Health, whereas driving requires the sharpest of reflexes. Cognitively speaking, anesthesia can slow reactions and other thought processes and can even contribute to temporary memory loss or impairment. Accordingly, it's almost a certainty that you won't be able to drive yourself home from a procedure in which you've been given anything but the most local of anesthesia. Further, the restriction on driving may continue for at least 24 hours after surgery. However, in some cases, your restrictions on driving may extend much longer.
After some surgeries, you shouldn't drive for weeks
If your surgery involves general anesthesia, you will most likely be told not to drive until you no longer feel groggy and the medications used to put you under are presumed to have left your system, per Healthline. However, in a number of circumstances, you won't be allowed to drive for quite a lot longer than that — for your own safety and that of everyone else on the road's. It depends upon the type of surgery. For example, if you've had any surgery that interferes with the mobility of your driving leg(s), you won't be given medical clearance to drive for a period of weeks, and possibly until your doctor has seen you and personally signed off on your physical fitness to drive, according to Dr. Joseph McCormick (via Orthopedic and Sports Medicine Specialists).
But it's not just your legs that your doctor is concerned about. Safe driving also requires the full use of your arms, shoulders, neck, and trunk. So, for example, since breast cancer surgery may involve lymph nodes taken from under the arm, it's typical for driving to be restricted for a week to 10 days after a mastectomy, per WebMD. If you left the hospital with surgical drains still in place, you probably will be told not to drive until the drains have been removed (via Breast Health Institute Houston), and that can take anywhere from one to five weeks (via UC Davis).
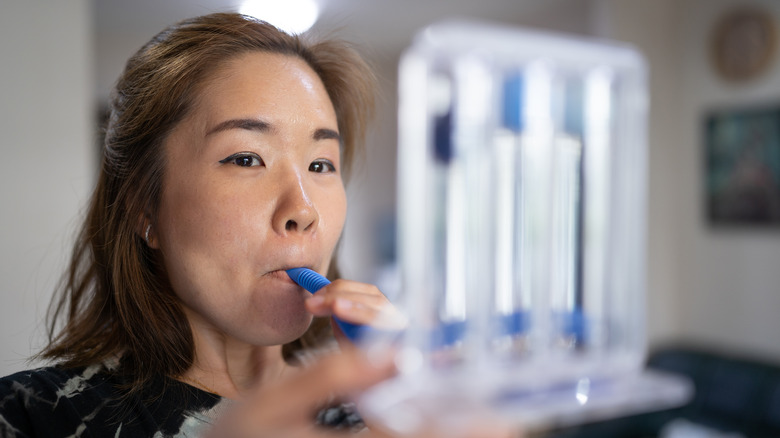
Don't skip the breathing exercises your healthcare professional prescribed
If you've had surgery that directly affects the respiratory system — including heart, lung, or abdominal surgery — then your surgical team likely prescribed any number of post-surgical breathing exercises, per Penn Medicine. The reason, as you might imagine, is that any such surgery can make breathing and clearing the lungs feel uncomfortable for a time. Problems arise when that discomfort leads you avoid breathing deeply or coughing, which can cause mucus to collect in your lungs, in turn raising your risk of infections such as pneumonia, per Dr. Andrew Chung (via Health Pages).
However, this is actually true of any surgery involving general anesthesia, according to Dr. Chung. This is because the drugs that are used to sedate you also slow your breathing and make your breaths more shallow. This has the effect of flattening the air sacs in your lungs, which makes it harder to take in deep and satisfying breaths immediately after surgery.
"In order to get air back into these sacs and open them up, you need to take deep breaths and hold them," Dr. Chung advises. To help you stay on top of your breathing exercises, many hospitals provide what's called an "incentive spirometer," a mechanical contraption that provides observable feedback as you breathe. The long and short of it: If you're given breathing exercises of any kind after surgery, it's in your best interest not to skip them.
Never smoke cigarettes after having surgery
If you're a smoker, your doctor has probably already urged you to quit, especially if you've been planning a surgery. If you haven't listened, you may be disappointed to learn that even if you have been smoking right up until your surgery (which you shouldn't have been, because that is also problematic, according to the World Health Organization), you will be strongly encouraged not to smoke in the aftermath. First, as a general matter, smoking stresses the heart, affects blood flow, increases blood pressure, and puts unnecessary stress on the lungs, according to Queensland Health. All of this is problematic in and of itself, but it also has the effect of reducing oxygen levels throughout your body, which is basically the opposite of what you want for your body when your body is trying to heal (per University of Iowa Hospitals & Clinics), not to mention trying to ward off post-surgical infections.
As World Health Organization (WHO) explains, smoking as little as a single cigarette "distorts a patient's immune system and can delay healing, increasing the risk of infection at the wound site." Smoking after surgery can also make pain more stubborn to treat, according to FootCareMD. The bottom line is that you should never smoke while you're recovering from surgery — whether or not your doctor knows you're a smoker and has the opportunity to warn you in advance.
Don't go back to your normal diet too quickly after surgery
Most people head into surgery on an empty stomach because doctors instruct patients not to eat or drink anything in the hours leading up to surgery — this is both to keep you from becoming nauseous, and to help keep your lungs clear of food and drink, per UCLA Health. But if you have a surgery scheduled that involves anesthesia, your surgical team will likely restrict your eating and drinking in the hours following your surgery as well. As registered nurse Jennifer L.W. Fin points out at Health Grades, "Your healthcare team wants to be sure that your digestive system is functioning well before you start eating solid food," and while it's important to drink some water to prevent dehydration once your IV fluid tube has been pulled, you should not "guzzle," but rather sip slowly to make sure your system is able to accept fluids by mouth without causing gastrointestinal distress.
As you resume eating solid foods, it's still a good idea to avoid foods that may cause digestive issues such as constipation (cheese, for example) and gastrointestinal discomfort (fried and fatty foods, for example). Additionally, registered nurse Jennifer Whitlock points out via Verywell Health that what you do end up eating and drinking can make your recovery smoother because your body leans on certain nutrients in healing itself (for example, protein). Accordingly, you should avoid foods with empty calories in the aftermath of any surgery. Here are some foods you should eat after surgery, and some foods you shouldn't.
You shouldn't drink alcoholic beverages after surgery
You may emerge from surgery feeling so relieved that it may seem that a celebratory drink is in order. However, you should not be drinking alcoholic beverages in the aftermath of a surgery because it may increase the length of your recovery, according to the professionals at Specialty Surgical Center. First, alcohol may weaken your immune system, which can increase your risk of post-operative infection. Second, alcohol can cause swelling in the body, which may interfere with the healing process, especially at the surgical site. Moreover, alcohol is dehydrating, which is not in your best interest after any surgery, according to registered nurse Jennifer L.W. Fink (via Health Grades).
Finally, since alcohol has a depressing effect on the nervous system, it should never be taken with prescription pain medication. For one thing, alcohol can interfere with how your body processes any anesthesia drugs remaining in your body. Further, combining the two can interfere with your cognitive functioning and even slow down your breathing to what Fink says could be "potentially dangerous levels."
Don't skip the antibiotics you may be prescribed
All surgeries present some risk of infection at the incision site, per Healthline, which says these are known as surgical site infections, or SSIs. In addition, all surgeries involve some degree of risk of what is known as a healthcare-associated infection — which include SSIs as well as various infections that may be picked up as a result of simply being in a place where numerous people are being treated for various ailments, according to the Joint Commission Center for Transforming Healthcare. The most common healthcare-associated infection is a urinary tract infection arising from the placement of a catheter, according to Cleveland Clinic. The second most common is an SSI, per the Joint Commission Center, which says that SSIs account for 22% of all healthcare-associated infections among surgical patients.
Post-operative infections are so common that WHO has been working to come up with guidelines for clinicians to reduce not only their frequency, but also the patients' risk of death (SSIs alone account for 8% of all deaths due to healthcare-associated infections, per the Joint Commission Center). Although post-operative prophylactic antibiotics are not necessarily the current standard of care, they are still recommended after certain surgeries and in certain circumstances. So if your surgeon recommends antibiotics, you shouldn't skip them just because you're feeling well or out of fear that you may be contributing to the development of related super-bugs.
Don't skip any probiotics you may be prescribed
Probiotics are a source of good bacteria that can help your body to fight infection and rebalance your body's bacterial flora after infection or antibiotic use, which can help you feel well and stay healthy, according to Cleveland Clinic. Some surgeons recommend the use of probiotics after surgery to help bolster the immune system against post-operative infections, to accelerate healing, and to prevent stomach distress that may be caused by antibiotics prescribed prophylactically, according to Logansport Memorial Hospital. But this is by no means universal, according to Cleveland Clinic, which says that in some cases, probiotics may actually cause infection or antibiotic resistance, among other things.
Nevertheless, probiotic use has been shown to reduce the incidence of a healthcare-associated infection known as "c. diff," which is short for clostridium difficile, by as much as 50% in high-risk populations, according to a 2018 study published in Current Opinion in Gastroenterology. The c. diff infection causes severe intestinal inflammation, and symptoms include severe, watery diarrhea, cramping, and wasting — and in some cases, it can prove fatal (per WebMD). Only your surgical team will be able to determine if you're at high risk for c. diff, or if you are otherwise a good candidate for taking post-surgical probiotics. If probiotic therapy is recommended for you, it's best not to skip it.
Don't put undue stress on your incision
Your surgical incision will be held together with sutures. However, a number of factors can contribute to your incision re-opening, which can put you at risk of infection, among other things. According to Healthline, some of these include health issues such as obesity, diabetes, high blood pressure, and other conditions that may negatively affect circulation. In addition, incisions made in connection with certain types of surgery, including surgery in connection with colorectal cancer, are at a greater risk for "dehiscence" (which is the clinical name for an incision opening after surgery).
However, dehiscence can also occur as a result of straining, including while coughing, sneezing, vomiting, or trying to pass a bowel movement, per Verywell Health. While you can't completely avoid any of these actions, nor should you, you can minimize the risk by bracing yourself while doing so. "Bracing your wound can help to prevent your incision from opening after surgery," Verywell Health advises. You can brace your wound by mimicking the action of hugging a pillow — or by actually hugging a pillow, if you have one handy. You can also do your part to avoid constipation by eating foods that are high in fiber, avoiding foods that are known to be binding, and by staying hydrated.
Don't work out until your doctor gives you the okay
Your doctor may recommend that you begin moving almost immediately after surgery — for example, in the form of breathing exercises, per Penn Medicine, or in the form of walking short distances, per Verywell Health, which can, among other things, help prevent deep vein thrombosis and pneumonia, as well as help get the digestive tract moving again. However, that does not mean that you should get back to your pre-surgery workouts just yet.
"It's an issue if you get active too quickly," according to Jonathan Whiteson, director of cardiac and pulmonary rehabilitation at Rusk Rehabilitation Center at NYU Langone Medical Center, per WebMD. Not only is there a risk of falling and becoming injured as a result, it's also possible to re-open your incision due to lifting weights or otherwise putting strain on your incision and sutures. Your doctor will recommend how much you should be moving based on the type of surgery you had, your age, your general health, and other factors, and you should heed those recommendations. In any case, "don't overdo it because you will have setbacks," according to general surgeon Greg Saggio (per WebMD).
Don't go back to work too quickly
Even minor surgery puts extra demands on your body, which will need time to rest and recover, per Occupational Health Consultancy. Not only does that mean you shouldn't get back to exercising before your doctor clears you to do so, it also means that you should carefully consider how much time you will need to recover before returning to work — as in, what you do to make money. First, going back to work may expose you to pathogens that can cause infection. Additionally, going back to work outside the home may subject you to physical activity that goes beyond what your doctor has recommended for you.
Further, as rehab specialist Jonathan Whiteson notes, you may not be mentally or cognitively ready to return to the demands of your job. "I've seen plenty of people try to do work while they're still in the hospital — with a computer and cell phone," he pointed out to WebMD. "They're not coherent, let alone able to make good decisions." Pearl Recovery Retreat & Wellness concurs on this point, explaining "after surgery, you're not in peak physical or mental condition, so the quality of your work is likely to suffer."
Don't skip post-surgical rehab
Rehabilitation refers to "a set of interventions designed to optimize functioning and reduce disability in individuals with health conditions in interaction with their environment," according to Physiopedia. Most post-surgical rehab begins right in the hospital (via Peake Physical Therapy), but in many cases, rehab may continue for weeks and months after surgery. And the longer it continues, the more tempting it may be to quit prematurely. But please don't.
Post-surgical rehab in the form of physical therapy, occupational therapy, speech therapy, and even cognitive behavioral therapy, is meant to address whatever it is your surgery may have taken from you, even temporarily, according to the Bella Vista Health Center. That includes regaining muscular strength, movement, and flexibility, as well as practicing methods of performing your day-to-day tasks in ways that will promote healing, reduce pain, and possibly prevent further medical intervention. In addition, for many people recovering from surgery, it can be difficult to know how much activity is too much versus too little, and one of the benefits of rehab is that it can help structure a balanced return to activity in the days and weeks following surgery.
Never ignore pain
You should expect some level of discomfort after a surgery, but if your pain increases rather than decreases over the course of your recovery, you should not ignore it, according to registered nurse Elizabeth Hanes, via HealthGrades. First, pain and the inflammatory response that it triggers in the body may actually interfere with the healing process and increase the risk of post-operative complications, according to a 2017 paper published in the Journal of Pain Research. If your pain is not under control, you may not be able to do the things you need to do that will help you to heal and prevent complications, Cleveland Clinic explains.
Of equal importance, pain is often an important signal from the body; after surgery, it may be your first symptom of a post-operative infection that demands prompt intervention, according to Hanes (via HealthGrades). Accordingly, Hanes urges surgical patients not to "feel weak or embarrassed" by concerns about pain and to speak up about it.