UTIs Explained: Causes, Symptoms, And Treatments
When things go wrong down there, it is common to feel embarrassed. A frequent suffer of urinary tract infections told Vice, "[Doctor's] questions – 'Are you having a lot of sex? Do you pee after sex?' – felt judgmental, and it was as if being unwell was my body's way of making moralistic comments about my sex life."
The stigma — if it causes people to delay seeking treatment — is damaging. Germs that cause infections creep into areas of the body where they don't belong and cause chaos. And while there are certain actions we can take to help reduce the likelihood of catching any illness (like regular handwashing), nobody who is sick deserves blame. We don't shame those who suffer from chronic sinus infections or contract the flu. Yet when our reproductive organs become involved, a whole new feeling is stirred. The truth is, anybody with a urinary system can catch a UTI. In fact, Martha Medina and Edgardo Castillo-Pino put this point front and center in their piece in the journal Therapeutic Advances in Urology. They state, "[UTIs] are the most common outpatient infections, with a lifetime incidence of 50−60% in adult women." And failure to address a UTI can have serious complications.
This article breaks down everything you need to know about UTIs, from the germs that cause them to the kinds of medicine that end them. Hopefully, you can feel a bit more comfortable addressing this major cause of discomfort.
Risk factors for UTIs
An article in Therapeutic Advances in Urology notes that women suffer the majority of UTI cases, and that this risk increases with age. "The prevalence in women over 65 years of age is approximately 20%, compared with approximately 11% in the overall population." Additionally, research shows that anywhere between 50% and 60% of adult women will contract UTI at least once in their lifetime.
In a way, this is a real estate problem. Biologically female reproductive and urinary organs sit in close proximity to the anus, which is a home for many species of gut bacteria. When these organisms stay in their neighborhood, all is well. But sometimes, they hitch a ride to the urethra and set up shop. Because the penis sits further away from the anus, it is more likely to be spared from contamination, which explains the UTI gender gap.
Meanwhile, another piece published in Therapeutic Advances in Urology cites several other risk factors for developing a UTI, including "frequent intercourse, vulvovaginal atrophy [after menopause], change of the local bacterial flora, history of UTIs ... family history, and a nonsecretor blood type..." Further, the authors state that any change in bladder function that occurs in one's lifetime — from urinary incontinence to medical interventions like urinary catheterization — increase risk.
Prevention of UTIs
Proper hydration isn't just for the athletes in Gatorade commercials. Keeping the body properly pumped with liquids is important for urinary health. Hydration helps our kidneys function properly as they produce urine. As the Mayo Clinic states: "Drinking water helps dilute your urine and ensures that you'll urinate more frequently — allowing bacteria to be flushed from your urinary tract before an infection can begin." The article also stresses the importance of emptying one's bladder after engaging in sexual intercourse.
Further, the methods we use to clean ourselves after a bowel movement can have a big impact. The Mayo Clinic recommends wiping from front to back. "Doing so after urinating and after a bowel movement helps prevent bacteria in the anal region from spreading to the vagina and urethra." An improper wiping technique, such as going from back to front, may allow normal gut bacteria such as E. coli to enter the urinary tract.
A common misconception is that the vagina requires deep cleaning. However, adding feminine products to your routine may actually cause more harm than good. Deodorant sprays and feminine care products like powders and douches may cause irritation in the urethra. Further, these products may disrupt the vagina's delicate pH balance and normal flora, giving invaders an environment in which to thrive.
Red flag symptoms
It's worth noting that the symptoms of a UTI are shared by many other urologic conditions. That is why it is important to have your symptoms evaluated by a medical professional. Clinicians are equipped with tests and expert training in finding a diagnosis. Forgoing treatment or trying to self-treat may lead to unintended harm.
The Urology Foundation lists several symptoms that are an immediate cause for alarm. If you are experiencing any of the following, it may be time for an evaluation. They include the inability to urinate, painful urination, visible blood in the urine, frequent urination, burning and lack of bladder control. These symptoms, while associated with UTIs, are also found in other conditions like cancer, kidney stones, enlarged prostate, and kidney infection. As the article states, "Sometimes these red flags are false alarms, but it is always a good idea to visit your [PCP] if you have any concerns."
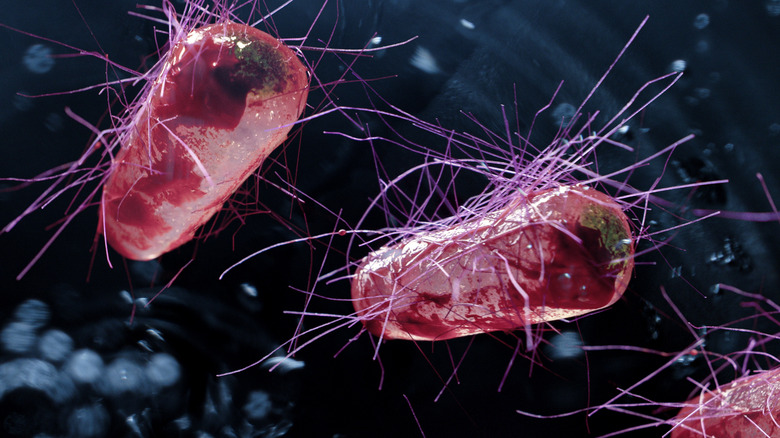
Germs that cause UTIs
According to a paper published in the National Review of Microbiology, "The most common causative agent for both uncomplicated and complicated UTIs is uropathogenic Escherichia coli (UPEC)... followed in prevalence by Klebsiella pneumoniae, Staphylococcus saprophyticus, Enterococcus faecalis, group B Streptococcus (GBS), Proteus mirabilis, Pseudomonas aeruginosa, Staphylococcus aureus and Candida spp." These species can also be found in the normal microbiota of the colon. Intuitively, this makes sense. UTIs are commonly the result of fecal contamination of the urinary tract. So, just as there isn't one predominant species of bacteria living in the colon, UTIs can also be a mixed bacterial bag.
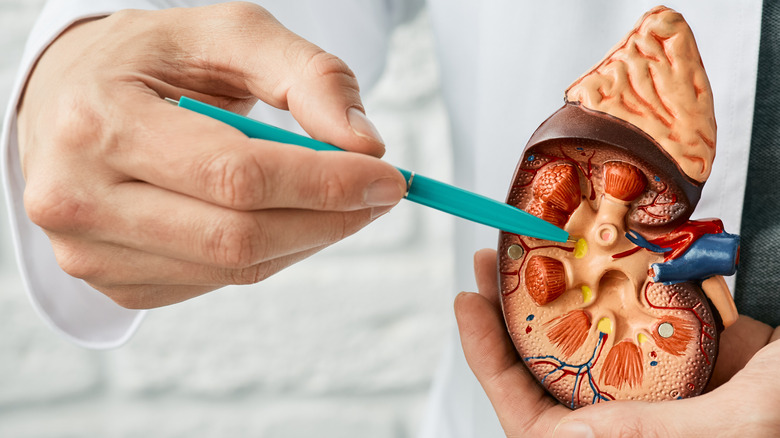
The real danger comes if one or more of these bacteria is allowed to take root in the urinary tract, forming a sticky colony of bacteria called a biofilm. Bacterial biofilms "produce toxins and proteases that induce host cell damage, releasing essential nutrients that promote bacterial survival and ascension to the kidneys." In severe infections that reach the kidneys, bacteria continue to damage healthy kidney cells, leading to colonization and, if they cross the kidneys' tubular epithelial barrier, bacteraemia.
And while UTIs can be treated with antibiotics, there's also the danger of increasing resistance to these medications. Thus, there's a growing need for "rationally designed and alternative treatments" for UTI.
Considering alternative causes for symptoms
We place a high value on making a specific diagnosis. This is understandable, since there's a lot of glory in guessing correctly. But medical professionals are trained to always consider an alternative explanation for the clinical picture in front of them. This is called a differential diagnosis. By forming a robust differential diagnosis, the clinician is afforded the benefits of the process of elimination. It is a critical tool in obtaining a complete history during a medical visit.
For example, if you are experiencing burning urination (a common symptom of a UTI), it is important to keep the horizon broad, says the American Academy of Family Physicians. Chances are, a UTI is the cause. The article notes that when a woman presents with painful urination, "[UTI] is the most common cause..." However, it also states that the differential diagnosis should be broad. Painful urination can be explained by UTIs, sexually transmitted infections, medication side effects and anatomic abnormalities.
Complicated vs. uncomplicated UTI
As mentioned prior, a major reason UTIs must be taken seriously is due to the risk of developing sepsis or blood infection. Once in the blood, these germs are tough for the body to get a hold of, leading to rampant infection present in many parts of the body.
While any UTI can lead to sepsis, the presence of certain conditions makes this more likely. If one or more of these factors is present in a patient's history, the UTI is classified as complicated. As a piece published in StatPearls elaborates, "Complicated urinary tract infections are those that carry a higher risk of treatment failure, and typically require longer antibiotic courses and often additional workup."
So, what makes the list? The article gives a long list, including infection in males or pregnant people and infection in the presence of urinary obstruction, immunocompromise, advanced age, or after medical procedures such as placement of urinary catheters.
Describing UTIs and common symptoms
UTIs are ubiquitous. The American Academy of Family Physicians (AAFP) states that most adult women will have at least one UTI in their lifetime. And while the discomfort alone is cause for concern, this problem costs our healthcare system an estimated $1.6 billion annually, accounting for near 7 million office visits.
According to the AAFP, in the eyes of a trained clinician, the presence of "classic" symptoms of UTI such as pain or burning with urination (dysuria), frequent urination, and an increased urgency to urinate can increase the probability of an infection by up to 50%. "The history is the most important tool for diagnosing acute uncomplicated cystitis, and it should be supported by a focused physical examination and urinalysis. It also is important to rule out a more serious complicated UTI."
In other words, if you are experiencing the symptoms described above, it's imperative that you consult a medical professional.
What to expect during your evaluation
Your visit to the clinic will begin with a medical history, physical examination, and urine test. Interestingly, discussing your history with a healthcare professional is a very important part of the process. As the AAFP explains, "A meta-analysis...found that the highest positive predictive value (PV+) of [UTI] in women was self-diagnosis." This means, if you believe you are having a UTI and say so, a competent provider is inclined to believe you. However, outside of self-diagnosis, the AAFP cites data saying that "the combination of dysuria and urinary frequency without vaginal discharge or irritation yielded a very high likelihood of UTI."
Physical exam is where some things can get a bit uncomfortable. Per the AAFP, "Often the most relevant findings on physical examination are sex-specific, including inspecting for infectious or atrophic vaginitis and STIs in women, and prostatitis and STIs in men." This means examination of the genitals may be necessary. This isn't always the case, though.
However, It is almost a guarantee that you will be asked for a urine sample, as it is the most useful test for patients experiencing painful or burning urination. Specifically, "the presence of nitrites [in the urine] is highly predictive of a positive culture." Thankfully, the urine dipstick can be done in the office, with results coming out in a matter of minutes.
Diagnostic testing
The urine dipstick has several areas that can change color in the presence of likely pathogenic chemicals in a urine sample. Mayo Clinic notes that the standard dipstick will measure urine's acidity, concentration, protein, and sugar levels. It also detects blood, ketones, bilirubin and infectious markers like leukocyte esterase or nitrites.
An article in the journal Clinical Infectious Diseases explains that nitrites can be found in a urine sample if bacteria are present. This is because some bacterial species break down nitrate chemicals into nitrites. However, nitrite testing has limitations. The article tells us, "[A] limitation to the test is that it requires testing a specimen of the first urine produced in the morning."
An accurate urine dipstick test also relies on the patient properly delivering the urine specimen, this is called the clean-catch midstream technique. Clinical Infectious Diseases explains, "...it is neither invasive nor uncomfortable, it is simple and inexpensive, it can be performed in almost any clinical setting, there is no risk of introducing bacteria into the bladder by catheterization, and there is no risk of complications." However, contamination from the vagina or skin flora may yield false results.
The specimen collected at the time of examination may be sent to a laboratory for culture and sensitivity testing in order to isolate the specific bacterial species responsible for the UTI.
First line medications
Once a UTI is diagnosed, antibiotic medication will likely be recommended. However, specific antibiotics only work on the bacteria they are designed for. Further, each drug behaves differently in the body, leaving clinicians with many options for treatment of UTIs based on each specific patient's situation. As an article from StatPearls elaborates, "Choosing an antibiotic depends on its effectiveness, the risk of adverse effects, resistance rates, and propensity to cause collateral damage; furthermore, physicians should consider cost, availability, and patient factors, such as allergy history."
Chances are high that the first medicine you will be prescribed will be either Macrobid, the sulfa-drug Bactrim, Fosfomycin, or a fluoroquinolone like Cipro of Levaquin. These drugs are commonly recommended as the first line of treatment. However, it's important to note that "there is no single, best agent to treat acute uncomplicated cystitis."
Most patients will begin feeling relief within 36 hours of starting antibiotics. That said, just because symptoms disappear does not mean it is safe to stop taking the medicine. Failure to complete the entirety of a prescribed course of antibiotics increases the risk of breeding antibiotic-resistant bacteria. A course of treatment for uncomplicated UTI commonly lasts from three to five days.
Treating men and pregnant women
Sometimes, the presence of other conditions in a patient's history excludes them from taking the first line medications or, due to complicating factors, require longer courses of treatment.
Regarding the treatment of complicated UTIs, there are no definite guidelines that apply for all treatments. However, therapy usually takes about seven days to be fully effective. A UTI in a man is automatically considered complicated, necessitating close monitoring for complications. However, men may still be treated with first-line medications like Cipro or Bactrim. The duration of treatment is recommended to be extended from three to five days to a course lasting from a week up to 10 days.
A UTI during pregnancy is also considered complicated. Pregnant women are unable to take many kinds of medicine, including several classes of antibiotics. Because of this, it is incredibly important for pregnant women to only take antibiotics prescribed specifically for their UTI. That means any leftover antibiotics in the medicine cabinet must be avoided. Regarding pregnancy, the StatPearls article says, "A shorter course of antibiotic therapy is preferred in pregnant patients." Additionally, common UTI medicines like fluoroquinolones and Macrobid are not safe for pregnant women. Instead, treatment relies on beta-lactam antibiotics such as Augmentin, Keflex, and cefpodoxime lasting from three to seven days, depending on the medication chosen.
Seeking further treatment
While most UTIs may be treated in the outpatient setting, an article from StatPearls explains that during certain occasions, hospitalization may be necessary to ensure the infection is cleared. Chief among these reasons are signs of severe infection, including failure of outpatient treatment, signs of septic shock, kidney damage or abscess formation in the urinary tract. The presence of one or more of these increases the risk of organ failure and/or death, and must be handled in the hospital to ensure patient safety.
Further, the symptoms of UTI may sometimes be so severe that hospitalization may be recommended, so that supportive medications can be administered alongside germ fighting antibiotics. Persistent nausea and vomiting, along with severe or unrelenting pain, may warrant a trip to the emergency room.
Patient specific factors may also make hospitalization a good idea. This includes patients who have difficulty managing their own care. This may be due to memory problems, cognitive changes, weakness, or other conditions. UTIs commonly cause confusion and altered mental status in older adults, making it difficult for these patients to follow the necessary instructions to recover.
Recurrent UTIs
For an unfortunate few, UTIs may repeat themselves several times over the years. Though they may consider this to be a nuisance, these people can take solace in the fact that recurrent UTIs "aren't likely to be the result of anything you've done" (per Harvard Health Publishing). In other words, some women are simply more prone to experience recurrence. These patients may be advised to alter their lifestyle to decrease the risk of developing future UTIs. This includes hydration, non-spermicidal contraception, emptying the bladder after sex, and topical estrogen therapy for post-menopausal women.
However, lifestyle changes alone aren't enough for those who deal with recurrent UTIs. The most important thing to do is to schedule a visit with your clinician to come up with a plan that will work for you and your specific needs. Typically, the article adds, this may include administration of low-dose daily antibiotics "for 6 months or longer".
Potential complications from UTIs
While the majority of people will fully recover from a UTI in a matter of days, some serious complications may occur, according to the Mayo Clinic. The article notes that having "two or more UTIs in a six-month period or four or more within a year" increases the risk of developing recurrent infections. Additionally, permanent kidney damage can occur if a UTI is left untreated. In men, UTI may lead to a stricture or narrowing of the urethra.
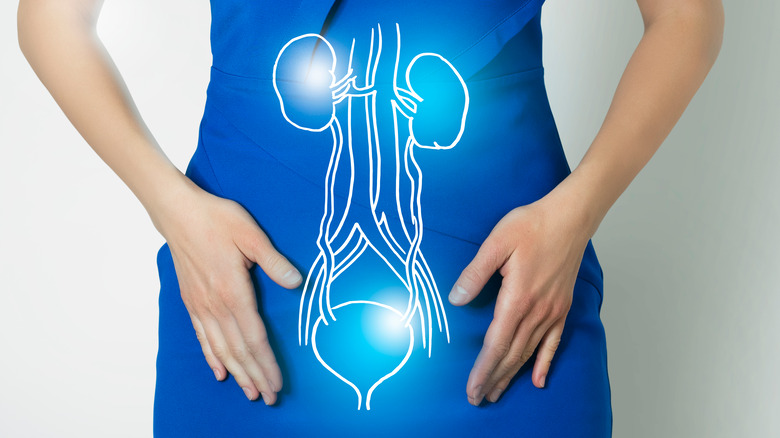
Perhaps most critically, there is a possibility of sepsis if a UTI goes untreated or is particularly strong. This may occur "if the infection works its way up your urinary tract to your kidneys." Anatomically, this makes sense. A pair of hollow tubes called ureters connect the kidneys to the bladder, allowing urine to be drained from the body (per Healthline). So, sepsis is possible if an infection that begins at the urethral opening travels up into the bladder, ascends to the ureters, infects the kidneys, and spills into the blood. If not promptly treated, sepsis is life-threatening.