What You Probably Never Knew About Pharmacists
Your pharmacist knows whether you prefer Ambien over Lunesta. The wonderful folks behind the counter know how many bad colds you've weathered and when you got your last flu shot. But what do you know about your pharmacist? And what exactly is a pharmacist?
As Pharmacy is Right for Me explains — and as many a pharmacist would no doubt happily tell you — "Pharmacists are medication experts who enhance patient care and promote wellness." Aspiring pharmacists need to complete a Doctor of Pharmacy degree, which requires the equivalent of seven years of higher education in health care, science, and law (via U.S. Bureau of Labor Statistics). It must be from a program formally accredited by the Accreditation Council for Pharmacy Education. And before a pharmacist can obtain their license (which they cannot legally practice pharmacy without), they must also pass a licensing exam. All of this is to ensure, among other things, that the person to whom you're entrusting your information and your health is qualified and prepared. But that's just the tip of the iceberg.
There are several kinds of pharmacists
You may be most familiar with the kind of pharmacist who dispenses pills at your local pharmacy — and a great many fall into this category. However, there are other kinds as well. According to the U.S. Bureau of Labor Statistics (BLS), pharmacists fall into four general groups. The first, which BLS refers to as a "community pharmacist," dispenses medication, including some vaccines, at retail pharmacies. With a duty to advise customers about drug interactions and side effects, including with regard to over-the-counter drugs, this type of pharmacist is an important part of the cycle of patient care (via Pharmacy Times). So too is what BLS refers to as a "clinical pharmacist." In fact, clinical pharmacists may be even more involved in patient care since they work directly in the clinical setting to dispense medication and consult with patients. A clinical pharmacist may even be involved in medication recommendations before a prescription is issued by a doctor.
A "consultant pharmacist" is involved less with patients and more with caregivers and clinical executives, consulting on medications and pharmacy services in general, although occasionally consulting directly with patients. Finally, "pharmaceutical industry pharmacists" work behind the scenes, helping to design and conduct drug trials as well as advising on marketing and regulatory matters. In addition, some pharmacists use their knowledge to help develop the next generation of pharmacists. These are pharmacists who choose to work in the academic setting as professors of pharmacy.
Pharmacists ideally possess certain fundamental strengths
Pharmacists have a bright and stable career outlook, per the U.S. Bureau of Labor Statistics (BLS), which estimates the average salary for a U.S. pharmacist to be about $129,000 per year. So, who should become a pharmacist? Individuals most likely to excel as pharmacists possess an array of specific attributes. The first is strong analytical skills. Pharmacists "must be able to evaluate a patient's needs and the prescriber's orders, and have extensive knowledge of the effects and appropriate circumstances for giving out a specific medication," according to BLS. That brings us to communication skills.
Community pharmacists and clinical pharmacists interact with patients all day long, even if indirectly through their employees. Their directions and advice must be precise and clear, whether spoken or written. Although other pharmacists may have less contact with patients, their communications skills are no less important as they write reports, convey recommendations, and train their employees to do so as well. Speaking of which, pharmacists can also benefit from possessing good managerial skills, particularly in a retail pharmacy setting. Like any scientist, a pharmacist also needs a keen eye for details, which becomes particularly crucial to their role in preventing drug interactions.
Something else that comes in handy for a pharmacist is some measure of creativity, according to The Pharmaceutical Journal. This can be helpful in problem-solving.
Pharmacists were once almost indistinguishable from physicians
The first "prescription" was written — in stone — more than 4,000 years ago, according to Pharmacy is Right for Me, at a time when community medical "experts" were generalists. It wasn't until the Middle Ages in Europe that there came to be a distinction between prescribers of medicine (i.e., physicians) and suppliers of the raw materials with which the prescribers would make the medicine (i.e., herbalists), according to Britannica. By the end of the 17th century, it was becoming increasingly less common for physicians to make medications at all. Instead, the job came to be handled by apothecaries, the predecessors to modern pharmacists (a new term as of the middle of the 18th century, per Texas Tech University Health Sciences Center).
Although the job of the apothecary, and later the pharmacist, often involved operating a storefront — often with a soda fountain beginning in the 19th century — it also involved mixing medications and consulting with patients about prescription medications. By the middle of the 20th century, however, medications were increasingly mass-manufactured, and starting in 1951 federal law prohibited pharmacists from recommending prescription drugs, leaving that job solely to physicians, and affording pharmacists greater focus on safely dispensing medications to customers.
But by 2003, pharmacists were again being permitted to counsel patients on prescription medications. Today, several states allow pharmacists to prescribe medicine, some subject to additional licensing requirements, according to GoodRx, which says the role of pharmacists continues to expand.
Founding Father Benjamin Franklin is considered an inspiration to American pharmacists
Founding Father and one of the framers of the Declaration of Independence, Benjamin Franklin, pictured above, was a lot of things. These include humor writer, journalist, printer, publisher, scientist, inventor, and diplomat (via Britannica). And while Franklin gets the credit for inventing at least one patented medical device — the "flexible urinary catheter," which he invented to help make his brother, John, more comfortable while dealing with kidney stones – and despite that Franklin made many other important contributions to health and healthcare in America (via Pharmacy Times), he was not actually a pharmacist, notwithstanding persistent misapprehensions to that effect (e.g., YouTube).
That being said, Franklin is a hero among pharmacists, per Pharmacy Times, which refers to Franklin as a "Found Father of Pharmacy" both for his practical applications of scientific knowledge and, perhaps more significantly, for his having established the first hospital pharmacy in the U.S. (at the Philadelphia Hospital, founded in 1751 and still in operation today as the Pennsylvania Hospital). Among other things that Franklin helped pioneer was the notion of maintaining the "apothecary," as it was known then, as a separate entity from the hospital's clinical practice. That being said, one of America's first apothecaries had already been operating in Philadelphia since 1729, owned by Irish immigrant Christopher Marshall, whose "Marshall Apothecary served as a community pharmacy as well as a training ground for aspiring pharmacists," according to WellRX.
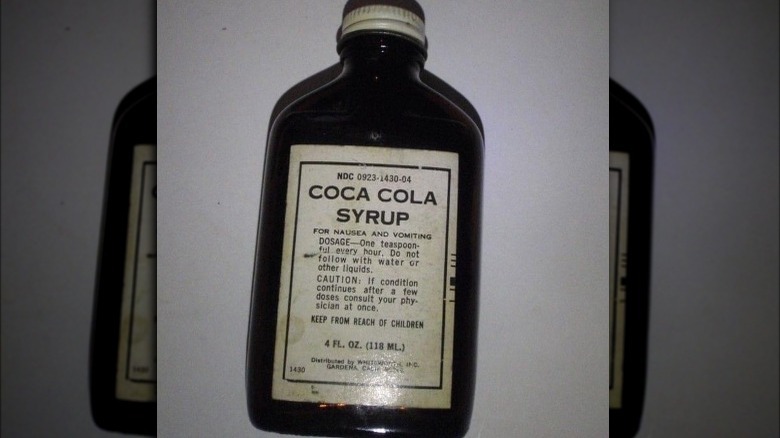
Pharmacists invented Coca-Cola and all these other things
When you think of a pharmacist, creativity may not be the first quality that springs to mind, but it's a useful attribute in the field. In fact, many things we take for granted today were first conceived in the mind of a pharmacist. For example, the friction match was invented in by a London pharmacist, John Walker, in 1827 (via The Pharmaceutical Journal). Other notable inventions by pharmacists include eyelash mascara, baby formula, margarine, and sunscreen (via The University of Sydney). And that's not including the many drugs that pharmacists are famous for having developed, including aspirin, penicillin, an early treatment for syphilis, and the rabies vaccine (via Pharmacy is Right for Me). Nor does it include Coca-Cola, Pepsi, or Dr Pepper, all of which were invented by pharmacists.
Pharmacist John Stith Pemberton invented Coca-Cola syrup and brought it to market in 1886, according to the Coca-Cola Company. The syrup was mixed with carbonated water to produce the "Delicious and Refreshing" taste that most of us have experienced at some time or another in our lives. In addition, the syrup (or a similar formulation) was sold as an over-the-counter remedy for nausea and vomiting until at least the mid-20th century (via Gale OneFile: Health and Medicine). Pepsi-Cola came along in 1893 thanks to the creativity of North Carolina pharmacist Caleb "Brad" Bradham (via Pepsi Born in the Carolinas). Dr Pepper soon followed, the brainchild of Waco, Texas pharmacist Charles Alderton (via The University of Sydney).
Pharmacist and serial killer: H.H. Holmes
Considering that the healthcare profession has the notions of "health" and "care" at its core, it might be surprising to learn that some of our nation's most notorious serial killers were healthcare professionals. These include, among many others, nurse and sanitarium owner Linda Burfield Hazzard, physician John Bodkin Adams, physician Harold Shipman, and, America's first serial killer, H.H. Holmes, who was a pharmacist by trade (via MDLinx).
Holmes, whose real name was Herman Mudgett, and who went by at least a dozen other aliases throughout his life, settled in Chicago in 1886 (via History). Initially, he worked at a pharmacy, but within months he became the owner. When Holmes was not working behind the counter, he kept himself busy with such sordid occupations as bottling tap water and calling it a health tonic, scamming insurance companies, murdering his girlfriends and selling their skeletal remains to medical schools for anatomy lessons, engaging in bigamy, and culling vulnerable tourists to the 1893 World's Fair in Chicago by offering them housing accommodations at the so-called "murder castle" he built adjacent to his pharmacy (via Biography). Of course, he didn't tell them it was a murder castle; those who found out, found out the hard way.
Holmes confessed to murdering 27 people, but he may have killed many more — or as "few" as nine before he was caught, tried, and subsequently hanged in 1886.
There's a really good chance your pharmacist is a woman
As of 2019, nearly 60% of all pharmacists in the U.S. were female, according to a report published by Data USA. To put that in perspective, consider that women comprised about half of all U.S. medical students that same year (via The Washington Post), and that women comprise a mere 37% of American lawyers as of 2020, according to Statista. The fact that the majority of pharmacists are now female represents a dramatic change from how things were as recently as the 1960s, when less than half of all pharmacy school graduates were female, according to Pharmacy Times.
In a presentation at the American Association of Colleges of Pharmacy Annual Meeting in 2019, pharmacist Suzanne Soliman attributed the evolution to "several factors," which include "an increase in chain and hospital pharmacies, a more hands-off climate, part-time flexibility, and substitutability." Nevertheless, "gender gaps still exist" throughout the profession. For example, as many as 10% of those who earn their PharmD are not currently working as full-time pharmacists. Worse still, most pharmacy owners, and all retail pharmacy chain CEOs, are men. And out of 143 accredited pharmacy schools, only 25 had female deans as of 2019. Gender inequality in the profession, notwithstanding women making up the majority of the workforce, was called out again in 2021 by the authors of an academic paper published in the American Journal of Health-System Pharmacy.
Your pharmacist has an elevated risk of substance abuse disorder
As may as 15% of workers in healthcare professions will "misuse drugs or alcohol at some point in their career," according to Pharmacy Times, but the rate is higher among pharmacists, among whom as many as one in 10 will deal with some form of full-blown substance abuse disorder at some point in their careers, according to Jeff Baldwin, PharmD, author and professor emeritus at the University of Nebraska Medical Center College of Pharmacy (via Pharmacy Practice News). Why are pharmacists at greater risk than other medical professionals?
If you guessed it has something to do with the fact that pharmacists have the most access to the most controlled substances, then you're onto something, according to Pharmacy Times. However, other factors play a role as well. These include workplace stress (which can be the case in any job, but easy access to opioids raises the stakes and the opportunity) and the glaring lack of "addiction education" that has been available to pharmacists. Further, Pharmacy Practice News cites "pharmacists' mistaken beliefs that their knowledge about medications" will somehow insulate them from becoming addicted. Accordingly, "shame" and a sense of personal isolation may exacerbate the problem for pharmacists experiencing addiction. Sadly, this adds up to a higher-than-average suicide rate among pharmacists, according to Houston Style Magazine, although the rate is higher among physicians.
If you or anyone you know is struggling with addiction issues or having suicidal thoughts, help is available. Visit the Substance Abuse and Mental Health Services Administration website, contact SAMHSA's National Helpline at 1-800-662-HELP (4357), or call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
The role of pharmacists in the nation's opioid crisis
Even while accounting for the devastating effects of the pandemic, the opioid crisis, which has killed half a million Americans over the last two decades, is still arguably the largest health crisis the U.S. has ever faced, according to The Commonwealth Fund. And it's only getting more serious. Whereas in 2015, 52,000 people died from drug overdoses, more than half of which involved opioids (via a 2018 paper published in Current Pain and Headache Reports), a preliminary report cited by the authors of a paper published in JAMA Network suggests that close to 95,000 people died of overdose during 2020.
A 2019 paper published in Pharmacy suggests that pharmacists may be able to play a role in mitigating the opioid crisis by offering such services as counseling on opioid use, storage, and disposal, and taking a more active role in prescription drug monitoring. However, pharmacists express "low confidence, time, and training" as obstacles to providing such service, suggesting a need for enhanced resources to be made available to pharmacists in this regard. For now, however, pharmacies are actually beginning to shoulder some of the blame for the crisis, according to News @ Northeastern. For example, at the end of 2021, a federal jury trial ended in the implication of Walgreen, CVS, and Walmart for "over-selling the benefits of opioid drugs and downplaying their negative effects" (via The New York Times).
If you or anyone you know is struggling with addiction issues, help is available. Visit the Substance Abuse and Mental Health Services Administration website or contact SAMHSA's National Helpline at 1-800-662-HELP (4357).
Your pharmacist is at a high risk for professional burnout, which can interfere with optimal patient care
Professional "burnout" has been a significant problem among medical professionals, and particularly among pharmacists, for decades, according to a 1990 study published in American Pharmacy, which identified women under the age of 40 working in a retail setting as being at heightened risk at that time. And it appears not much has changed in the intervening years: According to a 2020 academic paper published in U.S. Pharmacist, pharmacists in general now face one of the highest risks of burnout among healthcare professionals. The biggest contributing factors appear to be "time constraints and performance metrics," with the most significant attendant risk being negative outcomes for patients relying on their pharmacists to guide them toward safe prescription drug use in a diligent and energetic manner.
In December 2021, the American Pharmacists Association (APhA) warned readers that burnout among pharmacists is now approaching its "breaking point," in part because of the additional stressors brought about by the COVID-19 pandemic. Among other things, pharmacists shouldered much of the burden of both testing and vaccinating Americans. At the same time, pharmacists have been overburdened as a result of the labor shortage. In addition, pharmacists face unique challenges when it comes to getting paid by insurers for the clinical services they provide.
Strategies the APhA recommends for addressing this potentially dangerous situation include improving working conditions first by staffing adequately, thus enabling pharmacists to spend more time doing the job they were trained to do, which is safely dispensing medication and counseling patients.
COVID-19 has put pharmacists at risk for mental health issues
Professional burnout can put pharmacists in the precarious position of being unable to deliver the optimal standard of care required for safely dispensing medications to patients. However, the conditions that may lead to burnout among pharmacists, which have been exacerbated by reverberations from the COVID-19 pandemic, according to the American Pharmacists Association, may also lead to mental health issues among pharmacists. In fact, COVID-19 has taken a heavy toll on the mental health of pharmacists overall, according to a 2020 article published in the Journal of Pharmaceutical Policy and Practice.
Studies indicate that anxiety, depression, insomnia, and "traumatic distress" were reported by pharmacists during this time, with close to half of all pharmacists studied requiring some level of psychological support, according to Mena Alrais, PharmD (via U.S. Pharmacist). To put this in perspective, consider that studies show a "lower prevalence of psychiatric symptoms" among frontline physicians and nurses. Perhaps surprisingly, one of the most significant factors that comes into play is that in their day-to-day work, pharmacists tend to come into contact with more individuals than physicians and nurses, putting them at higher risk of exposure to the coronavirus. Here are some other unexpected effects that COVID-19 has had on mental health in general.
If you or someone you know is struggling with mental health, please contact the Crisis Text Line by texting HOME to 741741, call the National Alliance on Mental Illness helpline at 1-800-950-NAMI (6264), or visit the National Institute of Mental Health website.