Everything You Wanted To Know About Insulin
Chances are you've heard the word "insulin." Certainly, if you or someone you know has diabetes, you're very familiar with it. But there's far more to this seven-letter word than you might realize. For example, according to Britannica, it's specific cells in your pancreas that produce insulin, which is essential for keeping your blood sugar at healthy levels. Also, insulin wasn't always called insulin. One of the first people to identify it (a physiologist named Nicolas C. Paulesu) named it "pancrein."
Whatever its name, insulin began making headlines not long after it was "discovered." Or perhaps a better word is "extracted," since that's what scientists Charles H. Best and Frederick G. Banting achieved in 1921. As Britannica explains, these initial extracts were the first steps to creating injectable insulin to treat diabetes. And as a result, Banting, along with physiologist J.J.R. Macleod (who helped with them getting a "purified extract" of insulin), won the 1923 Nobel Prize for Physiology or Medicine.
Of course, with every scientific discovery comes new information that sometimes challenges previous findings. But with that said, insulin has remained an essential treatment of diabetes. However, that doesn't mean there's nothing new to say about this hormone — or for that matter, diabetes itself. Just the many ways it can be administered (yes, needles are no longer someone's only option) demonstrate how much we've learned about not just insulin but also our own bodies.
How insulin helps manage glucose
To really understand insulin, we need to first break down how it helps your body manage your blood sugar levels. As the Mayo Clinic explains, your body mainly depends on a type of sugar called glucose for energy. However, the body can't just manufacture glucose from nothing. It instead turns carbohydrates into this type of sugar. Now, you've undoubtedly heard the word "carbs" before, but as the Cleveland Clinic explains, carbohydrates are what's known as macronutrients (or essential substances or chemicals) that are found in foods and drinks that contain fiber, starches, and/or sugars.
According to the Mayo Clinic, the carbs you take in are turned into glucose and go into your bloodstream. And here's where your insulin comes into play. Although your blood provides an effective delivery system for glucose, without insulin, your cells wouldn't be able to absorb the glucose. Plus, you might not need all the glucose you produce at a given time. When this occurs, insulin helps your body store that extra glucose as glycogen in the liver.
To recap, without insulin, not only would your cells have a harder time getting energy, but excessive amounts of glucose would also circulate throughout your body. And as we're going to discuss elsewhere in this article, this can cause serious health problems.
Insulin resistance vs. prediabetes
Your cells need insulin to take in glucose for energy, but for some people, normal insulin levels aren't enough. As the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) explains, someone's liver, muscle, and fat cells might "resist" working with insulin, leading to them absorbing less glucose than another person's cells. This condition, called insulin resistance, can lead to the pancreas secreting larger amounts of insulin to compensate for these cells.
Now, the good news is that if the pancreas can keep up with this higher demand for insulin, then a person's blood glucose shouldn't exceed unhealthy levels. Unfortunately, when someone who is insulin resistant can't produce enough insulin to manage their glucose, this can lead to a condition called prediabetes. It's also possible to become prediabetic without first having insulin resistance if the cells in the pancreas that are responsible for making insulin cannot produce enough to manage glucose levels. Either way, a prediabetic's glucose will be higher than someone without prediabetes. And as its name suggests, prediabetes can eventually become type 2 diabetes.
While we can see a connection between insulin resistance and prediabetes, we're still not entirely sure why some individuals develop these conditions, according to NIDDK. But that doesn't mean we haven't noticed patterns pointing to possible risk factors, including family history, weight, high blood pressure, not exercising, and being 45 years old or older.
Type 2 diabetes
Once someone is prediabetic, they have larger amounts of glucose circulating throughout their body than they're supposed to, according to the Mayo Clinic. And this condition can eventually become type 2 diabetes, where not only is your body not making large enough amounts of insulin, but also your cells are resisting the insulin you have. This leads to higher amounts of glucose in your system.
Now, you might think that type 2 diabetes and its insulin-related issues would immediately cause severe symptoms throughout your body. However, it's possible for someone to have this condition and not even realize it for years. Red flags of type 2 diabetes like being hungry and/or thirsty often, feeling exhausted, or needing to urinate constantly could be attributed to other health problems. Additional signs can include one's feet or hands feeling numb, changes in vision, sores that take longer than usual to heal, and losing weight for no apparent reason.
Besides these external signs, type 2 diabetes can also have a negative impact on a person's organs, including their heart, and might increase the chances of developing other types of chronic diseases. And one more thing: The Centers for Disease Control and Prevention (CDC) explains that a woman who is pregnant might experience problems producing high enough amounts of insulin and develop gestational diabetes. While this condition typically goes away after giving birth, it can also increase the chances of developing type 2 diabetes.
Type 1 diabetes
While the pancreas is still making notable insulin if someone has type 2 diabetes (according to the Mayo Clinic), this isn't always the case for someone with diabetes. Specifically, if a person has type 1 diabetes, their body is making either no insulin or very small amounts, as the Mayo Clinic explains. And while type 1 was called juvenile diabetes because it tended to manifest itself early in a person's life, it's possible to develop it in adulthood.
Like other aspects of insulin-related health problems, we're still learning why someone develops type 1 diabetes, according to the Mayo Clinic. However, a common pattern is the immune system turns against the pancreas, attacking it and the cells that make insulin as if they were dangerous to the body. In fact, a possible reason why someone might develop type 1 diabetes is because of viruses invading their system. How far you live from the equator and family history can also potentially be risk factors for type 1 diabetes.
If your pancreas is producing either no insulin or very little insulin and you develop type 1 diabetes, you could experience changes in your appetite where you're far more hungry than normal. You also might become exceedingly thirsty, exhausted, and irritable. Other possible symptoms of type 1 diabetes include needing to urinate more often and blurry vision. And like type 2 diabetes, type 1 can have a negative impact on your organs like your heart.
Characteristics of insulin
For someone who doesn't have any form of diabetes and doesn't know someone who is diabetic, it might appear like there's one type of insulin that handles every need. But this is not the case. Yes, when a diabetic takes insulin, it's to help them compensate for their insulin issues. But as Endocrineweb notes, there's more than one kind of insulin, with different characteristics.
Before we explore the different types of insulin, it's important to understand its main three characteristics. According to the American Diabetes Association (ADA), different insulins can take a longer or shorter time to get into your blood and start reducing your glucose. This quality of insulin is called onset. Also, insulin isn't going to be at the same level of strength the entire time it's in someone's system. So another characteristic of it is when it is at its strongest or when its peak time is. Finally, even when a type of insulin is past its peak time, it's still working in your system. Because of this, we also measure it by its duration, or the total amount of time it brings down glucose levels.
Besides these characteristics of insulin, there's one more important aspect of it to keep in mind. Insulin cannot be taken in pill form because the digestive system would break it down before it had a chance to enter your bloodstream. This is why insulin injections are so commonplace.
Types of insulin taken before or with meals
Although there are three characteristics of insulin, that doesn't mean there are only three types. In fact, the CDC lists seven types of insulin, and a health care professional might prescribe a combination of different insulins based on factors like age and diet.
The first type is rapid acting insulin, which usually begins lowering glucose around 15 minutes after taking it. This form of insulin is usually at its strongest one hour after it enters someone's body, and continues to reduce glucose levels for two to four hours. Another type is rapid-acting inhaled insulin, which starts working 10 to 15 minutes after it's taken, is at its strongest 30 minutes after it enters the body, and works for three hours. Additionally, there's regular/short acting insulin, which starts working 30 minutes after entering the body, hits its peak two to three hours after being taken, and remains active for three to six hours. Also, while both rapid acting insulins are typically taken just before a meal, regular/short acting insulin is typically taken 30 to 60 minutes before a meal.
In addition to the seven types of insulin listed on the CDC's website, there's also ultra-fast acting insulins, according to the National Center for Biotechnology Information. As Healthline explains, these are typically taken with meals and begin working two to 15 minutes after entering the body. Their peak is 30 to 60 minutes after being taken, and they usually last four hours.
Types of longer acting insulins
While there are insulins that begin working quickly, there are also types that don't begin reducing glucose right away, but stay in your system longer (per Healthline). For example, intermediate acting insulin usually begins working two to four hours after being taken, peaks at four to 12 hours, and works for 12 to 18 hours. So rather than taking this insulin with or before a meal, it's taken once or twice daily instead.
Besides intermediate acting insulin, there's also long-acting insulin that begins lowering glucose levels two hours after it's taken and works for up to 24 hours. Additionally, there's ultra-long acting insulin, which begins working six hours after it enters the body and reduces glucose for at least 36 hours. Both of these insulins have no peak time and are only taken once a day.
In addition, there's premixed insulin that's a combination of short- and intermediate-acting insulin. This type, which is typically taken 10 minutes to half an hour before breakfast and dinner, can take anywhere from five minutes to a full hour to begin working and usually works for 10 to 16 hours. Plus, when it peaks can vary. And one more thing to keep in mind: As Healthline explains, even if a combination of any of the eight insulins mentioned in this article works well for you, it's not uncommon for you to need to adjust your insulin treatment plan periodically.
Insulin syringes
One of the most common ways to take insulin is to inject it. However, as Medical News Today points out, there is more than one medical device on the market for giving yourself a shot of insulin. For example, some diabetics use syringes, which come in different sizes (via the Better Health Channel).
Now, if you've never dealt with a syringe before, you might assume that a diabetic fills the clear area of it (known as the barrel) with insulin every time they need to take a shot. However, as Medical News Today explains, the barrel of a syringe like the types used by diabetics to take insulin have markings, which allow someone to measure out so many units of insulin. For example, they might need 30 units or 0.3 milliliters (ml), according to the Better Health Channel. Hence, it's not uncommon for a diabetic to have a syringe that can hold more units of insulin than they need to make, measuring out the correct amount easier.
Besides the barrel of the syringe, there are also different needle sizes for administering insulin. First, the needle is not supposed to penetrate the skin so deep that it goes into muscle. Second, the gauge or thickness of the needle is also important. Although thicker needles can hurt more, they also can help get insulin into someone's system more quickly.
Insulin pens
Besides syringes, insulin pens are also very commonly used by diabetics, according to Healthline. A big advantage to both reusable and disposable pens is the insulin is premeasured in the pen's cartridge.
Before using an insulin pen, you should go through a brief checklist. First, make sure you're using the right kind of insulin that hasn't expired. Additionally, check your insulin's appearance; it shouldn't be clumpy. Also, fast-acting insulin shouldn't have color to it and should be clear. You'll also need to prepare the pen. In general, you should roll the pen in your hands, but if you're using an insulin mix, you should also tilt the pen. You not only need to disinfect the top of the pen, but also attach a new needle each time you use it and make sure that there are no air bubbles in the needle by priming it. And even though some pens allow you to fix errors if you dial in the wrong amount of insulin, you should still be very careful with this step and double check the amount of insulin before you inject it.
Of course, these are just a few things to keep in mind when using an insulin pen. You should ask for full instructions from your health care professional who might have additional steps and reminders (like the angle at which to hold the pen's needle). Also, keep your insulin pens refrigerated before use.
Insulin pumps
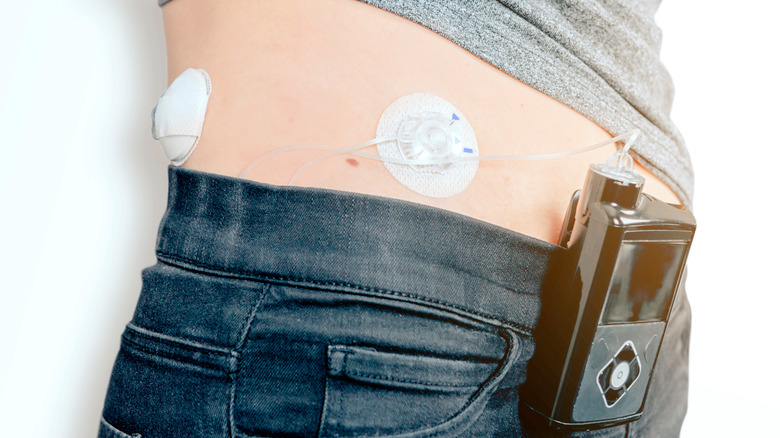
In addition to syringes and insulin pens, someone with diabetes can use an insulin pump. As Healthline explains, this means the person won't need to constantly stick themselves with a needle to take insulin. However, this doesn't mean that the insulin pump doesn't break the skin.
Like syringes and insulin pens, an insulin pump has a container that holds insulin. It also has a display screen and a tube called a cannula that acts like the needles in syringes and insulin pens (since it's inserted into the skin and allows the insulin to enter the body). However, unlike syringes and pens, insulin pumps can be programmed to give someone a certain amount of insulin. Plus, these pumps can give a diabetic the option of taking more insulin if needed. Additionally, some insulin pumps have the ability to monitor glucose levels and will stop sending out insulin if they detect someone's glucose drops too much. They also can be waterproof (to an extent), come with touch screens, and have wireless capabilities. And in the case of insulin pump patches, they're small enough to wear on your body against your skin.
Even though insulin pumps can do more than syringes and pens, they have limits. For example, as Healthline notes, a pump might alert a diabetic that their glucose is too high and give them the option to give themselves more insulin, but the device won't automatically increase the amount of insulin it's sending out.
Additional ways to administer insulin
As the American Diabetes Association (ADA) explains, insulin cannot be taken as a pill. But does it always need to be injected? Well, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), a diabetic can insert a short tube called an injection port into their skin. Then, when they need an injection, they can use the port instead of sticking themselves with a needle. Of course, they will need to change the port every few days, which does involve breaking the skin.
Okay, but are there any options that don't involve sticking something into your skin? According to NIDDK, jet injectors administer insulin via a high-pressure spray that penetrates the skin. Per WebMD, these devices are either spring-powered or air-powered. However, jet injectors are usually larger than insulin pens or syringes. They also tend to be pricier than insulin pens, and they don't have the same availability as other insulin-administering options. Additionally, there is a chance that a jet injector will make someone's glucose levels go too low.
In addition to jet injectors, there are insulin inhalers through which a diabetic can take insulin in through their lungs, according to the Mayo Clinic. However, there are a few things to keep in mind. When compared to some other insulins, inhaled insulin begins lowering glucose more quickly and has a shorter duration. Because of this, a diabetic might need to use both an insulin inhaler and an injectable longer-acting insulin.
Storing and disposing insulin
While there are a number of ways to take insulin, storing it is another matter. As the Diabetes Disaster Response Coalition (DDRC) explains, there are strict rules about how to store it and when you need to get rid of it.
Like other medical treatments, unopened insulin can expire, so the DDRC recommends always checking the expiration date. Also, it's important to store insulin at 36 to 46 degrees Fahrenheit. So yes, keeping it in a refrigerator works, but not in a freezer. In fact, the DDRC says that once insulin has been frozen, it's no longer usable. Okay, but what if you don't keep it in the refrigerator? Well, as the DDRC explains, insulin in vials or cartridges should be all right for 28 days, as long as they're kept at anywhere between 59 and 86 degrees Fahrenheit and aren't diluted or removed from the vial. Pump devices, however, are another matter. For example, if insulin is in the tubing of a pump device for 48 hours or was in temperatures higher than 98.6 degrees Fahrenheit, then dispose of it. And in general, it's important to keep insulin out of direct sunlight.
Of course, these are just a few rules for taking care of insulin, so you should speak with your health care professional about all the dos and donts for the particular types of insulin you're taking. Also, the DDRC recommends donating unopened insulin that hasn't expired to Insulin for Life.
Insulin rationing
Imagine that you need a treatment, but you're having problems paying for it. For some diabetics, this isn't a hypothetical situation. As Yale noted in 2018, the amount of money people here in the U.S. need to spend for insulin has doubled since 2008. This has led some to underuse their insulin to try to ration it, which can endanger their lives.
Researchers from the Yale Diabetes Center explored underusing insulin because of cost considerations and found that it goes beyond taking insulin less often or not taking the right amount of insulin for their needs. The individuals they surveyed also said they didn't refill their insulin prescriptions, stopped taking insulin at all, and even didn't beginning their insulin treatments. Unfortunately, as Dr. Kevin Codorniz, medical director of diabetes treatment at Loma Linda University Health in Southern California, told Men's Health, not properly keeping up with your insulin treatments can lead to strokes, kidney disease, amputations, and diabetic coma. You could also develop diabetic ketoacidosis.
According to the Cleveland Clinic, this condition comes with a number of possible symptoms, including difficulty breathing, vomiting, disorientation, and high glucose levels. In fact, elevated glucose or hyperglycemia can occur if you're a type 1 diabetic and give yourself too little insulin, according to the American Diabetes Association. So if you're having trouble affording insulin, don't ration it. Talk with your health care professional and your pharmacist. Also, there are resources available to help with insulin costs like getinsulin.org.
Other insulin-related health concerns
There's no denying that insulin is an essential treatment for diabetes. But just because taking insulin can help a diabetic compensate for insulin-related issues doesn't mean insulin has no side effects. Now, keep in mind there are different types of insulin, so their side effects might vary, according to Medical News Today. With that said, signs to watch for include depression, anxiety, and rashes in particular on the skin where one injects the insulin. In addition, they could gain weight for no apparent reason or cough when using an insulin inhaler.
Besides these side effects, insulin can also cause glucose levels to drop too low, a condition called hypoglycemia (per the National Institute of Diabetes and Digestive and Kidney Diseases). But hypoglycemia can also occur if someone takes insulin at a different time than they're supposed to, or takes a larger dose then recommended. Red flags someone is experiencing hypoglycemia include perspiration, exhaustion, and difficulty communicating verbally. They also might become confused, dizzy, or even unconscious. And in some cases, low glucose can cause seizures.
In addition to dropping glucose levels too much, Medical News Today explains that individuals who inject themselves with insulin can develop fat necrosis. According to the National Center for Biotechnology Information, if this occurs, then the person will develop a lump under their skin that can be painful. But if you're experiencing anything out of the ordinary regarding your health, you should speak with your health care professional.