What Is Myocarditis?
The heart is one of the most vital organs of the body. Without it, quite frankly, we would cease to exist. In the United States, nearly 1 in 4 deaths is due to some underlying form of heart disease (via U.S. Centers for Disease Control and Prevention). While high blood pressure, coronary artery disease, and heart attacks are the most common forms of heart disease, myocarditis is also a condition that affects the heart. Specifically, myocarditis refers to inflammation of the heart muscle, known as the myocardium (via Verywell Health).
There are several causes of myocarditis, some of which include: viral or bacterial infections (you may have heard of it most recently due to COVID-19 infection), systemic inflammatory diseases like lupus and sarcoidosis, radiation treatments, and even alcohol or illegal drug intoxication. Symptoms of myocarditis vary greatly depending on the length of time and the nature in which the heart muscle is inflamed.
Symptoms and diagnosis of myocarditis
People with a mild and acute case of myocarditis may not develop or experience any symptoms. In some cases, the condition is self-limiting and resolves on its own. If, however, a person experiences a higher level of inflammation within the heart muscle, they may experience chest pain, irregular heartbeat, palpitations, shortness of breath, lower leg swelling, fatigue, and more (via the Mayo Clinic). In the most severe cases, symptoms of heart failure develop.
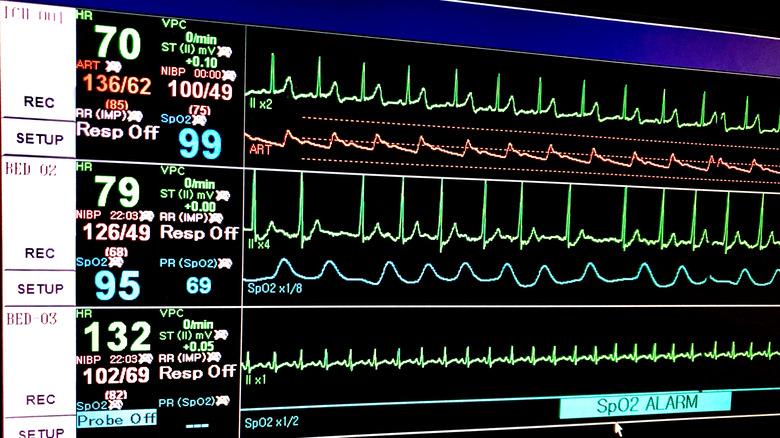
But how is myocarditis actually diagnosed? In addition to conducting a thorough history and physical exam, a healthcare provider may order specific blood tests, an electrocardiogram, and an echocardiogram (via Verywell Health). Blood tests, like the one that measures C-reactive protein (CRP), can be used to evaluate levels of inflammation, while cardiac markers can be ordered to rule out the possibility of a heart attack. An electrocardiogram, often referred to as an EKG, will show the electrical pattern of the heart, along with detecting any rhythm abnormalities. An echocardiogram is an ultrasound of the heart that can determine if there is fluid around the organ. It can also detect any damage or abnormalities of the heart structure, valves, or muscle.
Treatment of myocarditis
The most important aspect of treating myocarditis is determining the underlying cause. In many cases, myocarditis tends to be self-limiting and resolves on its own, especially when caused by a viral illness (via Johns Hopkins Medicine). If a bacterial infection has been identified, antibiotics help fight the infection and aid in the resolution and recovery. In people with systemic autoimmune or inflammatory illnesses, corticosteroids help reduce inflammation, but the systemic disease needs to be treated effectively in order to ensure a recurrence of myocarditis does not develop.
In certain cases of myocarditis, several heart and blood pressure medications can be used to reduce excess fluid surrounding the heart or the lower legs. They can also help regulate blood pressure and heart rate, and even help repair some of the muscle affected by myocarditis. These medications include diuretics, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and more. In very severe cases, more aggressive surgical intervention and management may be necessary.
If you or someone you know may be showing signs of myocarditis, it is important to speak with your healthcare provider or cardiology specialist as soon as possible.