Could Wait Times For Organ Transplants Soon Become A Thing Of The Past?
Researchers at University Health Network (UHN) in Toronto have created a proof-of-concept study that could significantly change how donor organs are given and received, according to U.S. News & World Report.
Currently, patients who need organ transplants rely on donors whose blood type matches theirs. According to Dr. Marcelo Cypel, senior study author and surgical director of the Ajmera Transplant Centre at UHN, patients with less common blood types are at an increased risk of dying while they wait for a match. In fact, patients with type O, specifically, who are waiting for a lung transplant have a 20% increased mortality rate, Aizhou Wang, first author of the study, said. Patients with rarer blood types wait years longer for transplants than those with more common blood types.
Based on this new study, however, researchers have discovered that by generating "universal" donor organs, they can decrease and possibly eradicate the wait time completely.
Converting blood types
Antigens are substances in the blood that trigger an immune response to viruses and bacteria that put your health at risk, according to Healthline. Antibodies are proteins made as a result of that trigger that attacks viruses and bacteria with the goal of removing them from the body. Blood type is determined "by the presence or absence of two antigens, A and B, on the surface of red blood cells," the American Red Cross explains.
There are four primary blood types: A, B, AB, and O. These primary groups are broken down into eight blood types, which depend on the absence or presence of Rh factor: A+, A-, B+, B-, O+, O-, AB+, and AB-. When it comes to donating organs and blood, compatibility matters (via National Kidney Foundation). Type A donors can give to type A and type AB recipients. Type B donors can give to type B and type AB recipients. Type AB donors can only give to type AB recipients. Type O donors can give to all recipients.
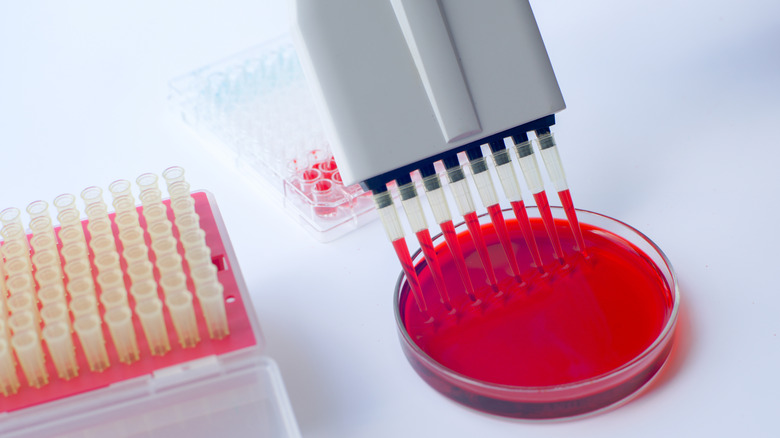
However, Aizhou Wang, first author of the new study, told U.S. News & World Report, "If you convert all organs to universal type O, you can eliminate that barrier completely." As part of the study, unsuitable lungs were treated with enzymes to "clear the blood type-determining antigens from its surface," U.S. News explained. A process called ex vivo lung perfusion was then used to add type 0 blood. In the end, "the treated lungs were well tolerated." A clinical trial proposal is now in the works.