A Complete Guide To COVID-19 Tests
We've reached a bit of an uncomfortable place in the COVID-19 pandemic. Lockdown restrictions are easing up and in-person events are happening again. It's also becoming socially normal to stop by and visit friends or family members. But all it takes is one case of COVID-19 to turn a dinner party or game night into a hotbed of viral spread. And then what happens when all of those infected individuals go out and spread it to the people they are with two or three days later?
Suddenly, as people are trying to adapt to a new normal, the question hangs precariously over everyone's heads: "Do I have COVID-19?" This explains why testing for COVID-19 has become such an important part of maintaining healthy communities and ensuring a safe, smooth transition back to everyday life.
Still, testing can be a tricky topic because there are so many different types of COVID-19 tests on the market, they have varying degrees of accuracy, there are different situations that call for testing, and there are different responses you should take depending on your results. So if you're feeling confused, here's a complete guide to everything you need to know about COVID-19 tests.
What is a COVID-19 test?
It can be pretty scary thinking that you might have COVID-19. After all, even though your own symptoms might be manageable at home, you could end up spreading the virus to somebody else who would be at much higher risk, such as an elderly person or somebody with a compromised immune system. So if there's a chance that you could have COVID-19 — either because you were around somebody who had it or because you're developing symptoms — the only way to find out is through testing.
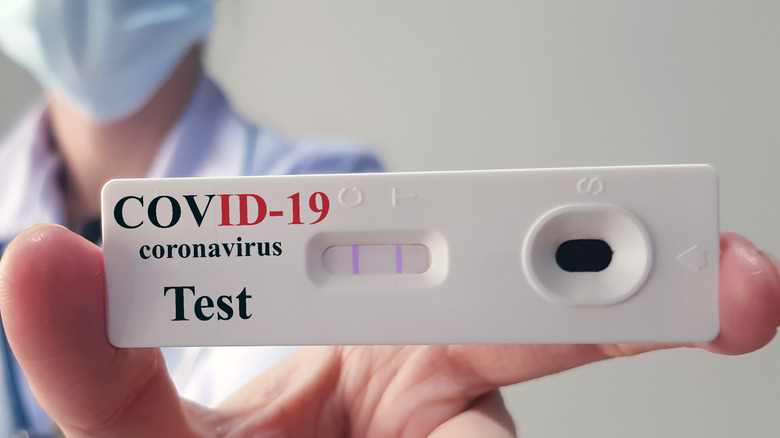
When people mention a COVID-19 test, several different methods might come to mind. But whichever type of test you end up using, the idea is the same: These tests determine whether you have either an infection of the novel coronavirus that causes COVID-19 or the antibodies your body developed either following an infection or after being fully vaccinated, as the Centers for Disease Control and Prevention explains.
A quick look at the different types of COVID-19 tests
There are different types of tests for COVID-19. You could test for a current infection, or you could test for antibodies (which indicate a past infection, but not necessarily a current infection). For this reason, an antibody test isn't the ideal option, according to the CDC. An antibody test, which may also be referred to as a serology test, does exactly what its name implies: It looks for the antibodies that your body develops to fend off the coronavirus. This means it's not a reliable indicator of whether you're currently sick or not.
By contrast, per the CDC, a viral test will tell you whether or not you're actually sick. There are two types of viral tests available. There are rapid tests, which can be done at home and can be purchased at a local pharmacy. These produce results in minutes. On the other hand, there are laboratory tests, which can take several days.
You should get tested if you were exposed to coronavirus or if you're showing symptoms
The two most important times for coronavirus testing are after a known exposure or if/when you're showing symptoms.
Imagine this scenario: You have a small get-together with a group of (fully vaccinated) friends at somebody's house on Friday night. By the time Sunday rolls around, you get a call from one of the attendees. Your friend started developing symptoms for COVID-19, so they took a test and it came out positive. But as of right now, you're feeling fine — so what should you do? According to the CDC, you should wait a minimum of five days after contact with the sick person before getting tested. Testing before that five-day minimum might result in a negative test because the infection has not fully developed yet.
In another scenario, you don't know of any recent exposure. However, you suddenly start to develop symptoms like a sore throat or a cough. Get tested immediately to confirm whether you have COVID-19.
Test results will help you determine whether you need to isolate or quarantine
A COVID-19 test can be the determining factor as to whether you need to quarantine or isolate. Although these terms are sometimes used interchangeably, it's important to understand the subtle difference between them. Per the definition of the Centers for Disease Control and Prevention, quarantine means to stay home and keep your distance from other people. Isolation is a stricter practice — an isolated person should stay away even from people in their immediate household, ideally staying in a designated sick room when other people are home.
Quarantining is for people who have been exposed to the coronavirus. It should be done for five days, and precautions (including wearing a mask and avoiding high-risk people) should be taken through the 10th day. Isolation is for individuals who have tested positive. If symptoms improve, a COVID-positive individual needs to isolate for only five full days, although precautions should be taken for the full 10 days. COVID-positive people who did not have symptoms need to isolate only for the full five days following their positive test. The CDC emphasizes that those who have a serious case of COVID-19 should isolate for a full 10 days.
By the time you test positive, it might be too late to prevent spread
Whether you get a rapid test or a lab test, it's an upsetting feeling to receive your results and see that they're positive — you have a case of COVID-19. And even if you're asymptomatic (that is, you feel completely normal and healthy), you could still potentially spread the virus to others who might get seriously sick. And as Huff Post explains, you've probably already been doing that by the time you test positive.
Yes, you read that right. Unfortunately, transmission is most likely to happen before your symptoms even start. And if your symptoms are what prompted you to get a test in the first place, that means you've been contagious for a couple of days already. How long, specifically? Most likely, you've been contagious for two days before developing symptoms and for two to three days following that. This also explains why CDC guidelines permit a return to normal activities five days after testing positive.
PCR tests might say you're positive when you've already recovered
"Hold up," you might be thinking. "Shouldn't I at least get a test that says I'm negative before I go back to my normal day-to-day activities?"
Well, depending on what type of test you take, you could end up testing positive even after you've recovered. According to Huff Post, PCR tests will continue to detect the virus in your body because this ultra-sensitive testing method looks for RNA from the virus in your respiratory system. This RNA can remain in your respiratory system for 90 days (yes, up to three months!) despite the fact that your body has, for all intents and purposes, fought the virus off. You're no longer feeling sick and you aren't contagious.
This is one situation where a rapid test could be more helpful than a PCR test. While a PCR's positive outcome doesn't necessarily mean you're a risk to others, a rapid test's positive outcome likely means you are. If you take a rapid test five days after developing symptoms and it says you still have COVID, that means you still have enough of the virus in your system that you could probably still spread it.
Testing is a crucial part of overcoming the pandemic
Don't underestimate the importance of testing. Having access to tests is not just beneficial for the person who is being tested — it's important for everyone around them as well. In fact, the National Institutes on Health consider testing to be just as integral in containing the spread of the virus as other measures like masks, vaccines, and social distancing.
As NIH explains, one of the hardest parts about the COVID-19 pandemic is the range and severity of symptoms that people can have from the disease. Many people who are infected by the coronavirus and contract COVID-19 might show mild symptoms or even none at all. But even asymptomatic individuals can transmit the disease, so getting tested will determine who needs to self-isolate to prevent the spread.
On an individual level, testing can be the difference between life and death for a person. If someone tests positive, they could get earlier access to treatment, which reduces their risk of severe illness, long-term symptoms, and death.
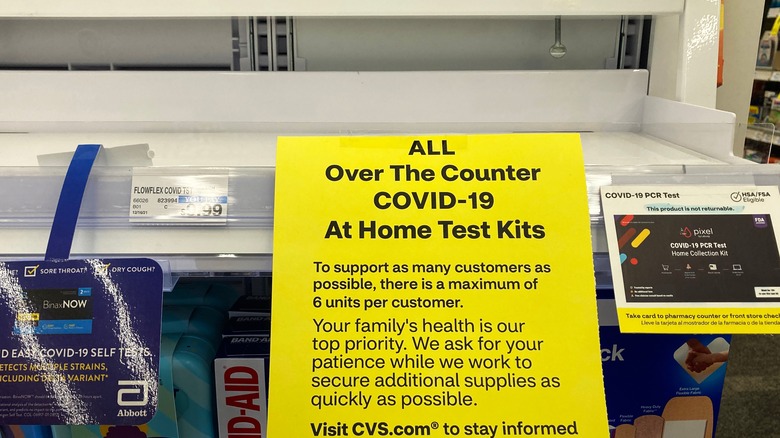
Demand for tests surged in December and early January, affecting supply and cost
The Omicron variant of the coronavirus created a spike in cases just in time for the holiday season. The sheer number of people with COVID-19 — along with those who were playing it safe while traveling, visiting family, or returning to work afterward — meant that testing was in high demand. The demand was so great that tests became pretty difficult to find, as NBC News reported. Test seekers were met with empty store shelves or long lines (and longer wait times) for lab tests.
Part of the problem was that tests had not been in such high demand during the months leading up to the Omicron spike. Manufacturers, retailers, and labs weren't prepared to provide as many as were needed in December and early January. In response, the federal government pledged $3 billion toward getting enough tests produced to meet demand, and manufacturers increased their output. For example, Abbott Labs went from making 50 million of its BinaxNOW at-home tests to 70 million tests.
The federal government is now providing free tests (and you can order them through the mail)
So tests are a crucial part of overcoming the pandemic, but tests can sometimes be hard to access? That sounds like a major problem. And it's one the federal government is aiming to solve by rolling out a program for free testing.
As CBS News reports, the Biden Administration recently announced that the government would provide four free at-home COVID tests per household. People can order their free tests at covidtests.gov and the tests will be delivered to them via first-class mail with the United States Postal Service.
Although that limit of four tests applies no matter how many people live in each household (in other words, a two-person household receives the same number of tests as a five-person household), the website provides information on where you can find testing locations in your area, as well as retailers where you can buy over-the-counter rapid tests.
Communities hit the hardest will receive priority when it comes to free tests
Unfortunately, not all communities have been affected by the COVID-19 pandemic in the same way. Both geographic and social communities see great disparity in terms of cases, hospitalizations, and deaths. The CDC even reports that communities of color are disproportionately affected by the pandemic when compared with white communities. Therefore, health equity must be a consideration when it comes to providing the resources people need to stay safe from the virus.
This is something the federal government is keeping in mind as it tries to provide free tests to communities across the country. As the White House expressed in an official statement, it is giving priority to the households that are most vulnerable. It is also working closely with organizations that serve groups like communities of color and people with disabilities so that those disproportionately affected by the pandemic know about the free tests and are able to access them easily.
You can also be reimbursed from your insurance company if you buy tests at a pharmacy
For most households, four free tests through the mail won't be enough to last them through the rest of the pandemic (even if there are fewer than four people within the household). But thanks to other efforts by the U.S. government, tests will still be easier to acquire. As The Hill reports, private insurance providers must now cover the cost of up to eight over-the-counter tests per person per month, either through reimbursement or by covering the out-of-pocket cost ahead of time.
Ideally, the insurance companies will cover the cost of the tests through the retailer, so the customer doesn't have to pay anything out of pocket. This is what the government is encouraging, according to CBS News. However, for insurance companies that are reimbursing their clients, receipts will likely need to be submitted. People seeking reimbursement from their insurance providers should hold on to everything associated with their tests, including both the receipt and the packaging. The law is effective as of January 15, 2022, so any tests purchased before that time will not be covered by insurance.
It's unclear whether insurance premiums will be affected by free test distribution
But here's one important possibility to keep in mind: Even though the eight COVID-19 tests per person per month are covered by your insurance, they might not end up being completely free.
As Kaiser Health News (KHN) explains, some private insurance companies may need to increase their monthly premiums to cover the cost of so many tests for their members. The total cost could end up reaching billions of dollars, depending on how many tests are actually bought and how many insurance members seek reimbursement.
Insurance companies ended up making a lot more money than they usually do over the past couple of years, because most people were staying home and putting off any elective surgeries they could. KHN explains that this increase in profit might explain why some insurance companies have not yet raised their premiums. However, members could expect to see price increases in the future.
People should choose whichever test is most readily available to them
Remember when vaccine distribution was still in its early stages? People were wondering whether there was an advantage in getting one manufacturer's vaccine instead of another one's? Now, people find themselves faced with a similar question when it comes to tests: Which type of test should I get, and is one type of test better than the other?
The short answer: Get whatever type of test is available (via NPR). Yes, there are slight differences between different tests. Rapid antigen tests are fast and convenient, while PCR tests are ultra-sensitive (and as already established, maybe a little too sensitive). Plus, there's the inconvenience of waiting for results from a PCR test when you might need to know urgently.
But despite all these variables, if you have symptoms or you find out that you were exposed, getting tested is better than waiting it out for a better test (and potentially getting no test at all). Rapid tests are not always accurate, but if you have symptoms and a recent exposure, it's safe to assume that a positive result on a rapid test is accurate — no need to get a more sensitive PCR test.
Remember, it's still possible to get a false negative
If you get a negative test result, that must mean you're in the clear, right? Not so fast. Unfortunately, it's still possible for you to get a false negative test result — and in the case of Omicron, that seems to be happening more frequently, as reported by NBC News.
There are several factors that seem to be linked to false negatives. Sometimes, it's because the person took the COVID test too early (before the infection really had a chance to develop). Additionally, asymptomatic infections tend to yield false negatives more frequently than symptomatic cases, so a person could have no signs of COVID-19, could test negative for it, and could end up spreading infection to others if they go about their usual activities anyway.
If you have been exposed to the virus but your test results are showing up negative, give it a few days before testing again. In the time that you're waiting, continue to take precautions as if you actually were sick, so that you don't infect others. Self-isolate if possible, and when you have to be around others, keep 6 feet of safe distance and wear your mask.