Uterine Fibroids Explained: Causes, Symptoms, And Treatments
Are you concerned about uterine fibroids? If so, you may be interested in learning more about their symptoms and causes, along with determining whether something needs to be done about them. According to the Cleveland Clinic, uterine fibroids are non-cancerous growths made up of muscle and connective tissue that can develop in or on the uterus. They are a surprisingly common health issue, with an estimated 40% to 80% of women developing fibroids at some point in their lives. Although all women can develop uterine fibroids, black women are disproportionately impacted (via Healthline). Additionally, age, genetics, and lifestyle can affect the risk of developing fibroids (via Verywell Health).
Medline Plus discusses several ways in which uterine fibroids can be problematic. Primarily, fibroids can cause a range of painful or otherwise undesirable symptoms, such as heavy, lengthy periods and severe menstrual cramps. These symptoms can make it difficult to go to work, participate in social engagements, or be intimate with a partner. In some cases, fibroids can also damage surrounding organs, impact fertility, and even lead to pregnancy complications. While treatment for uterine fibroids is not always necessary, those who are struggling with fibroid symptoms should know that there are both surgical and non-surgical treatment options available (via WebMD).
Uterine fibroids can cause a range of symptoms
Have you ever noticed that your period seems a lot worse than that of other women? Women with fibroids may quickly bleed through pads or tampons, experience debilitating cramps, and suffer from periods that seem to go on forever. If this sounds familiar, you may want to get checked for uterine fibroids. The Mayo Clinic states that common fibroid symptoms include heavy menstrual bleeding, periods that last over a week, pelvic pain or pressure, frequent urination, difficulty emptying the bladder, constipation, back pain, and leg pain.
Johns Hopkins Medicine explains that some women can also experience infertility, complications during pregnancy, and pain during intercourse due to fibroids. Additionally, excessive blood loss from heavy periods can lead to anemia, according to the Fibroid Institute of Dallas. Anemia is described as "a condition marked by shortage of red blood cells or dysfunctional red blood cells in the body" which can cause extreme fatigue, shortness of breath, and loss of energy.
Fortunately, not all women with uterine fibroids experience symptoms. A 2018 survey in Journal of Women's Health discusses the burden, prevalence, and treatment of uterine fibroids in the United States. Researchers observe, "Approximately 25% to 50% of women with fibroids are symptomatic, experiencing heavy menses, reproductive issues, pain, increased urinary frequency, and anemia." In other words, while some women experience a diminished quality of life due to fibroids, others remain completely unaware of their presence.
The most common fibroid symptom is abnormal menstrual bleeding
Although fibroids can cause many different symptoms, there is one that is more prevalent than the rest. A 2017 study in American Family Physician shares: "The most common symptom is abnormal uterine bleeding, usually excessive menstrual bleeding." However, as it is difficult to compare side-by-side with other women, you may not know whether your periods are normal or not.
Fortunately, the Mayo Clinic covers the differences between normal and abnormal menstrual bleeding. A normal menstrual cycle occurs between 21 and 35 days, then lasts between two and seven days. While periods can be irregular in the early years of menstruation, they usually shorten and become more regular as you get older. Also know that your period may be affected by some types of birth control like the pill and IUDs. It is important to consult your doctor if your periods stop (for more than three months) and you aren't pregnant, occur less than every 21 days or more than every 35 days, last longer than seven days, cause you to bleed through more than one pad or tampon every hour or two, or cause you to experience severe pelvic pain.
Symptoms can vary based on size, number, and location of fibroids
Not all women suffer from uterine fibroid symptoms. And when symptoms occur, they can vary from mild to severe. According to the Mayo Clinic, several factors can determine the severity of your symptoms, including the size, number, and location of your fibroids.
Uterine fibroids can range from the size of a seed to as large as a grapefruit, according to the New York State Department of Health. Small fibroids are less likely to cause problems. Of note, the largest fibroid ever reported was in 1888, when doctors removed a 140-pound fibroid from a patient postmortem (via CBS News.) Another factor: The more uterine fibroids present, the more likely it is that symptoms will occur. A woman can have a single fibroid or many of them, with the average number being six or seven when diagnosed (via USA Fibroid Centers). And Guinness World Records reports that the most fibroids ever removed was in 2016 — a whopping 186!
Finally, location can play a role in symptom development. Uterine fibroids are classified based on their location in or on the uterus, as well as by how they are attached to the uterus. There are four major types of fibroids: submucosal fibroids, intramural fibroids, subserosal fibroids, and pedunculated fibroids (via the Cleveland Clinic). "Submucosal fibroids cause issues with the reproductive tract, including heavy periods and trouble conceiving and carrying a pregnancy to term," according to Very Well Health. Subserosal fibroids tend to impact surrounding organs, such as the bladder and rectum. Intramural fibroids cause similar symptoms to submucosal and subserosal fibroids; pedunculated fibroids (attached by a stalk) can twist as they grow, leading to sharp pain.
The causes of fibroids are not entirely understood
While doctors don't completely understand why women develop uterine fibroids, it is widely believed that several potential factors are involved. These factors include genetic changes in fibroids, compared to "typical uterine muscle cells," hormones (like estrogen and progesterone), other growth factors such as insulin-like growth factor (IGF), and a substance known as extracellular matrix (ECM), which forces cells to stick together (via the Mayo Clinic).
There are a number of risk factors for uterine fibroids, including aging, genetics, and lifestyle. According to the US Department of Health and Human Services women most likely to be affected include those who are pre-menopausal, obese, have a family history of fibroids, are African American, have high blood pressure, or are deficient in Vitamin D. Pregnancy and long-term use of oral or injectable contraceptives may actually reduce your risk for developing these common growths. After menopause, research suggests that fibroids tend to get smaller; however, this is more likely to occur in white women than African American women.
Your doctor may recommend fibroid treatment
If you are experiencing symptoms of uterine fibroids, we recommend visiting your doctor as soon as possible to obtain an accurate medical diagnosis. Some fibroid symptoms can be similar to those of other, sometimes more serious health conditions. Heavy menstrual bleeding, for example, can also be a sign of hormonal imbalance — along with dysfunction of your ovaries, adenomyosis which "occurs when glands from the endometrium become embedded in the uterine muscle," an inherited bleeding disorder, or even certain types of cancer (via the Mayo Clinic).
If your doctor thinks you may have fibroids, they will probably first order medical imaging to confirm their diagnosis. According to Fibroid Institute Dallas, this is most commonly achieved with ultrasound, magnetic resonance imaging (MRI), or a computed tomography (CT) scan. Other options include saline infusion sonography and x-ray (via the US Department of Health and Human Services).
Once fibroids are properly diagnosed and assessed, your doctor will be in a much better position to discuss treatment with you. Whether treatment is ultimately recommended depends on a number of factors (via UCLA Health). These include whether or not you've had previous fibroid treatments, your age, the extent of your symptoms, fertility goals, the number of fibroids detected along with their size, and other health conditions.
Hysterectomy can be performed to surgically remove fibroids
Hysterectomy, the surgical removal of the uterus, can be used to treat uterine fibroids. It is the only treatment approach that is considered a permanent solution, according to a related blog by Mount Sinai Health System. So, while hysterectomy is highly effective, it also comes with some downsides and is not the right approach for everyone.
To begin with, hysterectomy is a major surgical procedure with inherent risks. Similar to other surgeries, these include blood clots, wound infections, hemorrhage, and even injury to the surrounding organs (via WebMD). Additionally, hysterectomy patients can develop complications. Some of these involve urinary incontinence, vaginal prolapse, vaginal fistula formation, and chronic pain. Next, some hysterectomies include the removal of the ovaries, which may result in the patient entering early menopause. As the New York State Department of Health discusses, early menopause can place you at increased risk for osteoporosis and heart disease, along with causing unpleasant symptoms like hot flashes and vaginal dryness.
Perhaps of greatest consequence, it is not possible to become pregnant after having a hysterectomy. If you are considering hysterectomy to treat your fibroids, be sure to carefully review all treatment options with your doctor.
Another type of surgery for uterine fibroids is myomectomy
Unlike hysterectomy which removes the entire uterus, myomectomy is a surgical procedure to remove only the fibroids from the uterus. According to the Mayo Clinic, myomectomy may be a good option if you plan to bear children in the future, your doctor suspects fibroids might be impacting your fertility, or you wish to keep your uterus.
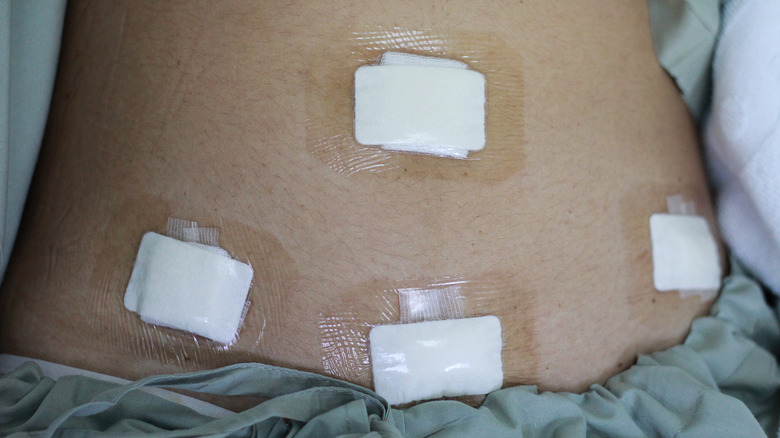
There are several types of myomectomy that can be performed. An abdominal myomectomy is the most invasive option and involves making an open incision to access the uterus and fibroids. Alternatively, a laparoscopic or robotic myomectomy (considered minimally invasive procedures) involves one or more small incisions in the abdomen through which a surgeon can insert instruments and remove fibroids, notes the Mayo Clinic. To treat smaller submucosal fibroids that bulge into the uterus, a hysteroscopic myomectomy may be recommended. This is when a surgeon accesses your uterus through your vagina and cervix, removing the fibroid(s) in pieces.
Myomectomy can alleviate fibroid symptoms, allow the possibility of future pregnancy, and leave your uterus in place. If you are having trouble conceiving due to fibroids, a myomectomy may even improve your chances of becoming pregnant (via the University of Michigan Health).
Surgery is not the only treatment option for uterine fibroids
While both hysterectomy and myomectomy can be used to treat fibroids, many women prefer to avoid uterine surgery altogether. Mount Sinai Health Systems discusses several potential non-surgical treatment options. The least invasive of these is watchful waiting, or delaying treatment, especially when a woman is approaching menopause. In this case, your doctor can monitor your condition over time to evaluate if or when your fibroids may benefit from treatment. If you are suffering from painful fibroid symptoms, using over-the-counter pain relievers like ibuprofen or placing a hot water bottle on your abdomen may help bring symptomatic relief (via WebMD).
Another non-surgical treatment possibility is drug therapy, which focuses on reducing symptoms and fibroid size. Mount Sinai explains: "Hormonal treatments such as oral contraceptives or a progestin-releasing IUD can help reduce heavy bleeding and pain. Gonadotropin releasing hormone (GnRH) agonists stop ovulation and the production of estrogen, and can reduce fibroid size."
WebMD also reports on two minimally invasive procedures that can be used to treat uterine fibroids. The first, fibroid embolization, aims to shrink fibroids by blocking their blood supply. The second, endometrial ablation, can be used to "destroy" the lining of the uterus. This method is sometimes used to reduce bleeding associated with small fibroids.
Uterine fibroids do not always require treatment
If uterine fibroid treatment doesn't sound like much fun to you, we certainly understand the sentiment. The good news is that not all fibroids require treatment. In fact, according to the American Society for Reproductive Medicine, "Fibroids usually do not require treatment because most patients with fibroids do not have symptoms." In addition, University of California San Francisco Health states, "Unless fibroids are causing excessive bleeding, discomfort or bladder problems, treatment usually isn't necessary."
If you have fibroids and choose to follow an approach of watchful waiting, it's important to continue to be medically monitored. During periodic visits, your doctor can review your symptoms, along with performing abdominal and pelvic exams to check in on fibroid and uterine size. Even if your fibroids continue to grow until menopause, this isn't necessarily a sign that intervention is required. Treatment is usually reserved for fibroids that significantly impact quality of life.
Fibroids can impact fertility and lead to pregnancy complications
If you desire pregnancy in your future, the presence of fibroids may be problematic. However, before panicking, you should understand that most women with fibroids can become pregnant and carry a healthy baby to term. Let's begin with some related statistics. According to a 2012 study in Obstetrics and Gynecology Clinics of North America, "Fibroids are present in 5% to 10% of infertile patients, and may be the sole cause of infertility in 1% to 2.4%." The study also informs us that fibroids can grow quickly during pregnancy, sometimes causing significant pain. After childbirth, fibroids usually shrink back in size.
Other problems that can arise during pregnancy with fibroids include bleeding, miscarriage, placental abruption (when the placenta separates from the uterine walls before delivery), preterm delivery (when a baby is born before 37 weeks), and increased risk for breech birth or cesarean delivery (via WebMD). If you have fibroids and wish to become pregnant, or are already pregnant and develop worsening fibroid symptoms, talk to your doctor about the best options for your individual situation.
Uterine fibroids may damage surrounding structures
Uterine fibroids not only lead to challenging symptoms, they can also cause damage to surrounding organs — the bowel, bladder, kidney, and stomach, for instance. Dr. John C. Petrozza, chief of reproductive medicine and IVF at Massachusetts General Hospital Fertility Center, explains, "If the fibroid is on the underside of the uterus, you could have constipation or pain when defecating" (via Everyday Health).
On the other hand, if your fibroid is growing toward the bladder, you may struggle with frequent urination. And if your ureter (the tube connecting your bladder and kidney) is impacted, urine can back up, causing kidney swelling (hydronephrosis) and damage. Another potential issue can occur when fibroids push on your stomach, making you feel full and experience abdominal swelling. This can lead to weight loss or, in some cases, cause a woman to appear pregnant.
Uterine fibroids can also "change the shape of the uterine cavity," leading to fertility issues. Brigham and Women's Hospital covers some of the reproductive complications that can arise from the presence of fibroids, including miscarriage, infertility, preterm labor, breech presentation, and problems during labor.
Fibroids can affect your sex life
Although this isn't as commonly discussed as other effects of fibroids, uterine fibroids can impact your sex life in several ways. To begin with, fibroids can cause pain or discomfort during sex, depending on their size and location (via Fibroid Treatment Collective). Additionally, heavy or lengthy periods can sap your energy, be messy, and not exactly leave you in the right mood for intimacy. If you struggle with frequent urination due to fibroids, this may be distracting at inopportune times. Finally, abdominal bloating or swelling due to fibroids can significantly affect body image and self-esteem. According to the Fibroid Treatment Collective, "A very large fibroid can even cause the uterus to expand to the size equivalent to a pregnancy heading into the 3rd trimester." This could be particularly difficult for women struggling with infertility.
Houston Fibroids covers three ways to make sex with fibroids easier. Along with openly communicating with your partner, they recommend focusing on foreplay so that you will feel relaxed and ready for intercourse. You and your partner can also try experimenting with different positions until you find a comfortable one. It may also be wise to look for alternate ways to connect as a couple when sex is too painful or undesirable. And we want to mention that while sex can be an embarrassing topic for some to discuss with a doctor, we encourage you to do so. Your doctor may be able to provide treatment that will help improve things — just be sure to ask about your full range of treatment options.
Uterine fibroids can take an emotional toll
Along with causing physical symptoms, uterine fibroids can also impact your emotional health. In fact, according to a 2015 study in the Journal of Psychosomatic Research, "Most participants exhibited a significant emotional response to their fibroids, including fear, anxiety, anger, and depression. Half of the women felt helpless and believed that they had no control over their fibroids. Many women possessed a negative self-image and cited concern over appearing less attractive, which led to difficulties becoming intimate. Several women felt that they lacked substantial support to help them deal with these issues." If you have concerns about your emotional health as a result of fibroids, we encourage you to reach out to your doctor for help.
In addition to the above issues, the vast majority of women with fibroids (90%) have concerns with the fibroid treatments they are offered, according to 2014 research published in American Society for Reproductive Medicine. And women, particularly those who are African American, also feel that they are not being offered their full range of treatment options. If you have similar concerns, consider seeking a second opinion.