Everything You Need To Know About Your Knees
While your knee joint is the biggest joint in your body, it's so much more than that. Each of your knees is complex junction of bones, muscles, tendons, and ligaments, plus special tissue for lubrication and shock absorption. Its hinge-like construction not only allows you to sit, walk, run, and jump, but the knee joint is strong enough to handle a force equal to double your body weight or more — four times as much while you run, for example.
You use your knees almost constantly, so it's easy to take them for granted. But knee problems are one of the leading causes of disability in elderly people. According to the American Academy of Orthopedic Surgeons, the disability risk for osteoarthritis of the knee is as high as receiving a diagnosis of cardiovascular disease. The knee might even be considered an organ — like the heart — and its failure causes serious health issues.
The knee is not only distinctive in its attributes — your knees are unique compared to everyone else's. One study found that when combined with other measurements, knee scans were 93% accurate in identifying individuals.
Knee injuries are common
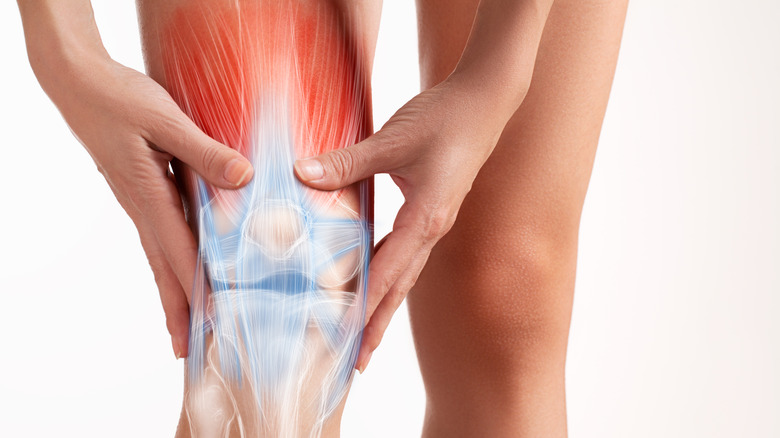
Your knee is prone to injury because it's big and, well, it's also complicated. Three bones come together at your knee: the femur (thighbone), the tibia (shin bone), and your kneecap, or patella. Lashing those bones together, you have a complex web of tendons, which attach muscles to bones, and ligaments, which hold bones together. All of this is surrounded by a capsule of connective tissue, which releases a fluid to keep the joint lubricated (via the Arthritis Foundation).
All of those parts can, and do, get injured by life's hard knocks. The most common knee fracture, or broken bone, is an injury to the kneecap, typically due to a vehicle collision or some other high–energy trauma. If the bones are knocked out of alignment, it's called a dislocation. Ligaments and tendons can be injured or torn by trauma to the knee, or by forcing the joint outside its comfort zone — changing direction rapidly, for instance, or landing from a jump incorrectly during a sport like football or basketball (via the American Academy of Orthopedic Surgeons).
Your best bet if your knees take a knock? Start with the RICE method — rest, ice, compression, elevation. See a doctor if it doesn't get better, or if the injury was accompanied by a popping sound, or if the joint can't move, is swollen, or is severely painful.
Different kinds of arthritis can affect the knee
The bones that meet in your knee are covered with cartilage, a connective tissue that provides a cushioning surface allowing the joint to move smoothly. Unfortunately, cartilage has a limited ability to heal. When it wears down or degenerates, the bones lose their cushioning, and the result is joint pain and stiffness of arthritis. The most common form of knee arthritis is osteoarthritis. It usually happens later in life, a consequence of wear and tear on the joint. Being overweight, or overusing your knees (for example, if you have a job that requires a lot of repetitive motion) increases your risk. A serious injury to the knee can also lead to osteoarthritis (via Hopkins Medicine).
Less commonly, the knee can be affected by rheumatoid arthritis. This is an autoimmune disease in which the body's immune system attacks tissue in the knee and other joints, breaking down cartilage. The cause of this isn't known. While cartilage damage can't be reversed, there are lots of options for managing an arthritic knee, including physical therapy, medication, lifestyle changes (fewer pick-up basketball games, more swimming), and surgery.
By the way, the old chestnut that someone can predict the weather from the way their arthritis acts up? There may be truth to that, since changes in atmospheric pressure can affect sensory nerves in the joints.
Bursitis can affect the knee
Here's a scene from an old-timey movie: It's raining. It's cold. And the chicken coop needs fixing. Suddenly, the main character blurts out, "I'll do it next week! My bursitis is acting up!" It may sound like a fake complaint, but it's a real thing. And bursitis can affect the knees and other joints.
Similar to other kinds of "itises," bursitis is an inflammation — in this case, an inflammation of fluid-filled sacs called bursa which cushion large joints like the knees, elbows, and shoulders. Overusing or injuring a joint can trigger this inflammation; for example, plumbers or other people who spend a lot of work time on their knees might get kneecap bursitis. Lack of stretching — or not warming up — before exercising can also cause bursitis of the knee (via Hopkins Medicine).
Symptoms of bursitis vary, but typically include pain, tenderness, swelling, redness, and trouble moving the affected knee. Usually you can turn this around by treating it like a sprain with the RICE method, followed by an OTC painkiller if you need one. More severe cases might require a steroid injection. But sometimes bursitis is caused by infection, in which case treatment might require antibiotics, and drainage of fluid with a needle or surgery. See your doctor for symptoms that don't improve, or if you have fever, chills, sweats, or symptoms other than pain or soreness.
Millions walk among us on artificial knees
Knee replacement surgery has been around since 1968, enabling people with joints damaged by arthritis or injury to resume activities that healthy-kneed people take for granted, like driving, climbing stairs, or walking. According to the American Academy of Orthopedic Surgeons, a more accurate term might be "knee resurfacing" surgery. The procedure removes damaged cartilage from the surfaces of the bones, and replaces it with a new surface of metal or ceramic — with a plastic spacer in between — that restores smooth and painless movement to the knee. A 2014 assessment found that about 4.7 Americans have an artificial knee, which adds up to 1.5% of the U.S. population.
Arthritis is the most common reason that people have the surgery, which can result in a significant reduction in pain and disability, reported the AAOS. Complications are uncommon, occurring in less than 2% of patients, and most people can resume their normal activity levels in three to six weeks. Physical therapy and specific exercises are required to help restore the knee's movement and strength. Most (90%) knee replacements still function after 15 years; a recent review found that 82% last for 25 years.
An artificial knee takes getting used to; it might produce strange sensations or even make noises. And it can set off metal detectors. On the plus side, here's an unexpected benefit: A study found that after surgery for hip or knee replacement, 42% of patients reported an increase in libido, and 41% reported more frequent sexual intercourse.
Knee injuries are more common among women
If you're a sports enthusiast, you've probably heard of an injury called an ACL tear — maybe you even suffered one yourself. This refers to damage to the anterior cruciate ligament, a band of tissue inside the knee that helps connect the thigh bone to your shin bone. The ACL is involved when you make sudden stops, jumps, or changes in direction, as in sports like soccer, basketball, football, and downhill skiing. Too much stress on the tendon can cause it to tear — typically with a popping sensation in the knee, followed by pain, swelling, and joint instability. Depending on the severity of the tear, the injury might heal with rest and rehab, or surgery might be required (via Mayo Clinic).
What you may not be aware of is that this type of injury is more common among women. Studies of college athletes have found that the risk of an ACL injury to be three to nine times greater for women than for men. Why the difference? Research points to both extrinsic (choices made by players and coaches) and intrinsic (biological differences between men and women) reasons. Hormonal and anatomic differences may play a role, but specialized training programs designed to prevent ACL injuries in female athletes have been found to decrease risk (via the International Journal of Sports Physical Therapy).
What your knees need
There's plenty that can go wrong with your knees — they're in constant use, after all, and have to handle a force equaling 150% of your body weight, or more. But there's also a lot you can do to protect them. If you're overweight, losing weight is the best gift your knees could get. Also, exercise will keep your knees healthy. If you already have osteoarthritis, exercising can reduce the pain.
When you exercise or play sports, warm up first and use proper form. It's also important to know what to do if your knee gets dinged. Get it checked out by a doctor after any accident or injury, especially if you can't bear weight on it, the pain is severe, your knee is visibly deformed or buckled, your knee is locked or you can't flex or straighten it, the area's warm, swollen or discolored, you have pain or other symptoms in your calf, the injury is followed by a fever, or symptoms haven't resolved after three days.
For knee pain that's not severe, try applying ice for 15 minutes per hour on the first day, and four times daily after that. Rest with the knee elevated to reduce swelling, and manage the pain with an OTC pain reliever (via National Library of Medicine).
Why is my knee so noisy?
When a joint cracks or pops, the phenomenon is called crepitus. Michael Stuart, professor of orthopedic surgery and co-director of sports medicine at the Mayo Clinic, told the New York Times that crepitus is very common. "Our joints make a lot of noise," he said.
Knees can get noisy because over time, the cartilage that covers your bones can become uneven, and their rough surfaces make noise when they glide over each other as the joint moves. Also, the ligaments that hold bones together can make noise as they tighten during movement. Sometimes gas bubbles build up in the fluid around a joint, making noise as they burst.
Those things are generally not concerning — they're "physiological," a consequence of how your body is put together. But when joint noises are accompanied by pain or swelling, or start happening after your knee has been injured, it's time to get the problem checked. You might have a tear in a meniscus, one of the shock-absorbing structures in your knee. Or it could be that the cartilage in your knee has been injured or worn down, causing arthritis (via WebMD).
Sometimes the problem with your knee isn't your knee
Pain is a sign of a problem, but it's not always a straightforward indicator of where the problem is. Sometimes the pain you feel in one part of the body is actually being caused by an issue happening in some other part of the body. Doctors call this "referred" pain.
One relatively common example of this is that osteoarthritis of the hip can cause pain that's perceived in the knee. Sometimes this is the only sign that there's a hip problem, which might go unnoticed if not evaluated by a orthopedic specialist who's familiar with the phenomenon. One study found that 47% of people with hip arthritis had pain at or below the knee. Referred knee pain can also be triggered by issues with your feet or ankles, since the way you walk affects your knee joint. Knee pain might also be caused by issues with the illiotibial band, a ribbon of connective tissue that stretches from your hip to your knee and helps you walk (via U.S. News and World Report).
Lack of sleep makes knee pain worse
Sleep is important for health — on par with exercising and eating a healthy diet, according to the American Academy of Sleep Medicine. One reason not to skimp on sleep is that lack of it seems to affect how your body processes pain. A study of more than 10,000 volunteers found that people who had insomnia performed 10% worse in a test of pain tolerance than people who got enough sleep. And the more often they had insomnia, the worse their pain tolerance was.
Osteoarthritis of the knee can be painful enough to make sleep difficult, and research suggests that this might make the pain feel worse. In one study, researchers tested the pain response of people who had knee arthritis, and found that the worse their quality of sleep was, the more sensitive they were to pain. Another study found that patients with osteoarthritis had sustained improvement in their pain — lasting as long as 18 months — if they got better sleep.
Acupuncture and tai chi can help knee pain
Osteoarthritis is the most common form of arthritis, and the knee is one of the most common joints to be impacted. So as you can imagine, there's been lots of research on a variety of treatment methods, both pharmaceutical and otherwise. In 2019, the American College of Rheumatology and Arthritis Foundation released guidelines for managing osteoarthritis. These guidelines emphasized a comprehensive approach to managing osteoarthritis of the knee, hip, and hand, using multiple treatment options with details determined by patients and their doctors.
Exercise was strongly recommended in the guidelines and, separately, tai chi was suggested as well (for the knee and hip). According to the report, practicing tai chi may help people with arthritis improve their strength and balance, decrease the risk of falls, and improve symptoms of depression. The report also gives acupuncture a "conditional" recommendation, meaning research points to a benefit, but it's not clear how big the effect is. Yoga was also given a conditional recommendation, since its use for managing knee arthritis hasn't been well-studied.
How to ID your knee pain with four questions
So your knee is hurting and you're not sure why. You gave it the classic RICE treatment (rest, ice, compression, elevation), but the problem hasn't gone away. What now? Your next step — maybe not literally, because ow — is to get to a doctor. According to the Cleveland Clinic, the two of you will get to the bottom of this mystery quickly if you can answer four important questions. Such as where does it hurt? Pain below or above the kneecap can be caused by the inflammation of a different tendon (tendonitis). Pain on the inside or outside of the knee might be a torn ligament or meniscus.
Also, it's critical to know what makes the pain better or worse? With osteoarthritis, the pain worsens during activity, sometimes getting worse as the day goes and as you become more active. Pain that's strong in the morning but eases with activity suggests inflammation or rheumatoid arthritis.
Another question your doctor is likely to ask: What does the pain feel like? If you can describe the quality of the pain, this can be a clue to the cause. A sharp, burning pain suggests an irritated nerve; a constant ache sounds more like arthritis. Finally, you'll want to know what else is happening. For example, does your knee make sounds when you move it? Does it get locked, or is your range of motion limited? Any symptoms that accompany the pain are important to note.
Someday cartilage from your nose could help your knee
In osteoarthritis, cartilage that lines the bones of the knee is degraded, causing pain and reducing mobility. Treatment options are limited to managing the symptoms, and replacing the damaged tissue with an artificial knee when the condition becomes severe. But recent research suggests that one day, damaged cartilage might be replaced with new tissue grown from cartilage samples taken from the patient's nose.
In animal studies, nasal cartilage was found to be capable of growing in the knee joint, and it seemed to counteract the inflammation of arthritis. When this approach was tested in two human volunteers with severe knee osteoarthritis, both of them reported a reduction in pain and an improved quality of life. No adverse side effects were reported.
Why take cartilage from the nose? Tissue grown from nasal cartilage cells seems to have regenerative properties that joint cartilage doesn't, the researchers noted in a press release from the University of Basel, Switzerland, where the research was conducted.
We're still making new discoveries about the knee
You might think there's not much new to know about the knee. But it was less than 10 years ago that scientists shed light on a knee enigma (known in the biz as a kneenigma) which was first suggested in the 19th century.
Surgeons in Belgium were investigating the outcome of injuries to the anterior cruciate ligament (ACL), a band of connective tissue inside the knee that can be torn in sports like soccer, football, and basketball, which place rotational force on the knee. Attempting to discern why some patients still had problems after the injury was surgically repaired led researchers to suspect the presence of an unidentified knee ligament — first proposed by a French surgeon in 1879 and not well-investigated since. By closely examining the knee structure of cadavers, they were able to identify and describe what's now known as anterolateral ligament (ALL).
The ALL is located on the side of the knee, connecting the thigh bone (femur) to the shin bone (tibia). It seems to help keep the knee from rotating, and damage to the ligament could be the reason why an injured knee sometimes remains unstable after a torn ACL is surgically repaired (via Live Science).
Ostriches are the only double-kneecapped animals
Ugh, ostriches. They just seem determined to prove how unique they are. Not only are they the largest birds on Earth, not only can they run at 45 miles per hour and kick you into next week as easy as look at you, but they're exceptional in another way: Ostriches are the only creatures in the entire animal kingdom that have two kneecaps on each leg.
It's not clear why these birds are so blessed. An investigation in which researchers scanned an ostrich leg to create a 3D digital model resulted in some interesting possibilities, but also raised more questions. The double-kneecap seems to decrease the force of the ostrich's leg muscles. However, it may also increase the speed with which the joint can move, granting the bird more speed. And it could provide protection for the leg's tendon as well. Sophie Regnault, lead researcher and Ph.D. student from Royal Veterinary College, told the Society for Experimental Biology, "Understanding more about different kneecap configurations in different animals could help to inform prosthesis design, surgical interventions, and even robots with better joints."