Can Intermittent Fasting Help With Diabetes?
Intermittent fasting is a type of eating plan in which you abstain from eating during a certain period of time ranging from 16-24 hours. For example, you may eat during an 8-hour window and fast for 16 hours. You can also fast certain days of the week. A popular alternate-day fasting schedule is a 5:2 schedule, which allows you to eat normally for 5 days and eat a restricted diet of a 500-600-calorie meal 2 days a week, per Johns Hopkins Medicine.
Intermittent fasting triggers a "metabolic switch" that helps the body and brain in several ways, including improved memory, heart health, and physical performance (per Johns Hopkins Medicine). The practice also helps to prevent obesity, which is a risk factor for diabetes — especially type 2 diabetes. Obesity causes inflammation in the body, which affects how the body produces insulin, according to Livestrong. If intermittent fasting can potentially prevent obesity, can it help with diabetes?
Intermittent fasting can benefit diabetics
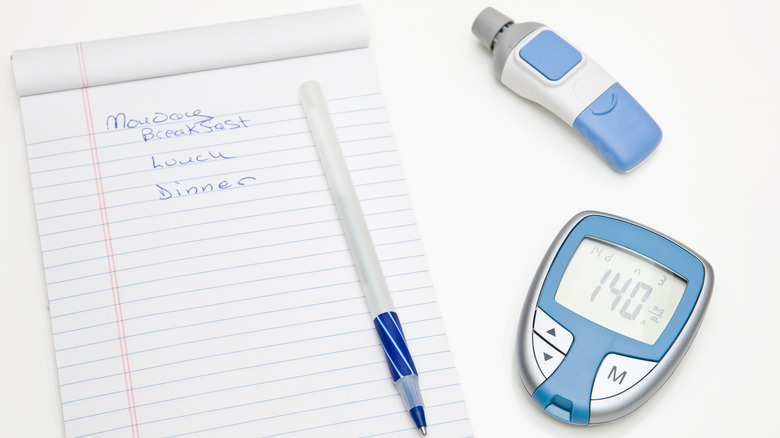
Simply put, diabetes occurs when the body is not able to metabolize insulin properly, creating an imbalance in blood sugar levels. Since intermittent fasting puts the body in a fasted state, there is no insulin in the bloodstream, allowing insulin levels to lower. A 2018 study published in Cell Metabolism indicated that people who fasted for several hours a day had "dramatically lower" insulin levels. Furthermore, research published in the Clinical Diabetes and Endocrinology journal suggests that intermittent fasting is an "effective non-medicinal treatment option for type 2 diabetes."
That is not to say that intermittent fasting will work for everyone. Healthline points out that the primary concern for diabetics when it comes to fasting is hypoglycemia (when your blood sugar drops too low) and hyperglycemia (when your blood sugar is too high). To be on the safe side, you should speak with your primary care physician before embarking on an intermittent fasting journey.