The Real Difference Between Being On A Ventilator And Being Intubated
Being intubated and being placed on a ventilator have one thing in common — nobody wants it to happen to them or anybody they love, but unfortunately, they have both happened to many people during the COVID-19 pandemic. While you may be familiar with the terms, you may be wondering what exactly is the difference between the two.
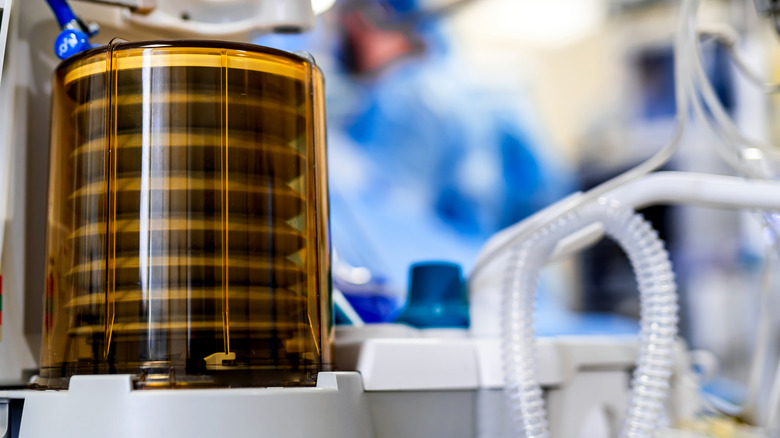
According to the National Institutes of Health (NIH), a person is put on a ventilator if they can't breathe and get enough oxygen into their blood. This can happen for a variety of reasons, such as stroke, pneumonia, sepsis, cardiac arrest, and acute respiratory distress syndrome. The ventilator will blow air into the patient's lungs. With the less-invasive method, breathing support will be provided through a face mask fitted tightly over the patient's nose and mouth.
If the patient's condition is more severe or if non-invasive ventilation isn't sufficient, they may need to be intubated.
Intubation often but doesn't always accompany ventilation
Intubation can happen for a variety of reasons, but when the purpose is breathing support, a tube is placed into the patient's windpipe and connected to a ventilator so that the ventilator can blow air directly into the person's body. The tube is typically inserted through the nose or mouth, but if the patient is expected to be on the ventilator for a long time, the doctor may perform surgery and insert the tube through a hole in the front of the patient's neck. Of course, anesthesia is used, so the patient is not awake or feeling any pain (per NIH).
There are some other reasons besides breathing support for which a person may be intubated. One example is nasogastric intubation, which is when a tube is placed through the mouth or nose into the stomach or small intestine. This may be done to pump out poison or provide nutrients to people who can't swallow (per Merck Manual).