Type 2 Diabetes Explained: Causes, Symptoms, And Treatments
According to the Centers for Disease Control and Prevention, more than 34 million Americans have diabetes. Approximately 90 to 95% of such ones have type 2 diabetes. Additionally, research has shown that one in three adults has prediabetes, but 90% don't know that they have it (via Healthline).
The primary reasons for the growing number of diabetes cases in the United States include the ballooning rate of obesity, including severe obesity, the lack of physical activity among adults and children, and increased consumption of carbonated beverages like soda, and high-sugar processed foods, according to MedicineNet.
Harvard Health revealed that people are being diagnosed with diabetes at younger and younger ages and more complications are arising. "These young adults possess high rates of obesity, smoking, and sedentary lifestyles, as well as high blood pressure and cholesterol (lipid) levels, all contributing to an earlier onset of complications," the publication detailed. The medical community also relaxed blood sugar targets to prevent dangerously low blood glucose levels in older adults. It's possible that this strategy was unintentionally lenient for younger adults. Insurance coverage and the skyrocketing costs of medication and insulin might also play a role in the increasing amount of complications.
Genetics and lifestyle factors are at play
According to Mayo Clinic, type 2 diabetes is the result of two interconnected issues. First, cells become resistant to insulin. Insulin is the hormone that is responsible for ushering glucose out of the bloodstream and into our cells. When the cells in muscle, fat, and the liver no longer recognize insulin, blood glucose levels rise. Simultaneously, the pancreas cannot produce as much insulin as we need to maintain normal blood glucose levels.
Having overweight or obesity is the biggest risk factor for developing type 2 diabetes, and if the fat is stored in the abdomen, the risk is even greater (via Mayo Clinic). Per WebMD, other risk factors for the development of type 2 diabetes include high blood pressure, elevated blood lipids (cholesterol and triglycerides), high-fat diet or a diet rich in carbohydrates, drinking excessive amounts of alcohol, and carrying a diagnosis of heart disease. A past diagnosis of gestational diabetes or giving birth to a baby weighing more than nine pounds can also increase your risk of type 2 diabetes.
Of course, there are risk factors that you have no control over, including being over the age of 45 and being of certain ethnicities, including African American, Native American, Hispanic American, or Asian American (via WebMD).
Proper nutrition and physical activity can often prevent type 2 diabetes
According to the CDC, being diagnosed with prediabetes can be a warning bell for many. It means that things can still be turned around to prevent or hold off the development of diabetes. Losing just 5 to 7% of your body weight (10 to 14 pounds for a 200-pound person) can drastically decrease your risk of progressing to full-blown diabetes.
By adopting a moderate exercise program (e.g., walking for a half-hour after dinner on weeknights), you can further reduce your risk. Being overweight increases the risk of developing type 2 diabetes by an amazing seven times, according to the Harvard T.H. Chan School of Public Health. Obesity increases the chances that you will develop the disease 20 to 40 times than your risk would be if you were of normal weight. Harvard explained that stronger muscle uses insulin more efficiently and removes more sugar from the blood. Because fat contains 9 calories per gram, while carbohydrate and protein contain around 4 calories each, cutting the fat from your diet is sometimes enough to encourage weight loss (via National Institute of Diabetes and Digestive and Kidney Diseases).
Mothers who have gestational diabetes need to be especially attentive to their lifestyle after giving birth. According to Everyday Health, 5 to 10% of mothers who have gestational diabetes will immediately transition into type 2 diabetes after giving birth. Additionally, between 20 and 50% will develop it over the next 10 years.
The symptoms of type 2 diabetes are easy to ignore at first
The symptoms of type 2 diabetes can be fairly benign at the beginning and include urinating more than usual, feeling thirsty and hungry even though you're drinking and eating enough, and feeling extremely tired without reason. The thirst and frequent urination occur because the kidneys try to excrete excess blood glucose from the body by increasing urination, which can, in turn, increase the risk of developing yeast infections (via Medical News Today). Hunger and fatigue are interrelated and occur because the cells can't access the glucose stuck in the blood to get energy from it. In essence, the cells are starving even though there's too much glucose in the blood.
Some people may also experience cuts and bruises that are slow to heal and tingling, pain, or numbness in the hands and feet, according to the American Diabetes Association. Both the impaired healing and the symptoms in the hands and feet occur because of nerve damage, and blood circulation issues brought about by hyperglycemia (via Medical News Today).
Some individuals develop a condition known as acanthosis nigricans, which causes patches of dark, velvety skin to form on the creases of the neck, armpit, or groin of individuals with obesity and insulin resistance. However, acanthosis nigricans has other, less common, causes, including other health conditions such as Cushing disease or treatment with certain medications (per DermNet NZ).
The complications of untreated diabetes can be life-threatening
The complications of untreated or poorly treated diabetes are myriad, as pointed out by the Cleveland Clinic, including slowed stomach emptying (gastroparesis), eye problems, foot, and leg ulcers, gum disease, hearing problems, sexual dysfunction, skin conditions, and urinary tract infections. People with diabetes are more likely to develop heart disease, kidney disease, strokes, and liver disease, including nonalcoholic fatty liver disease. Most of these issues are caused by the havoc that glucose wreaks on blood vessels and nerves throughout the body.
As described by the CDC, diabetes complications cluster together because they often share the same risk factors and feed off one another. For example, individuals with diabetes and high blood pressure have an especially high risk of eye and kidney disease, and smoking doubles the risk of heart disease in people with diabetes.
Some people with diabetes experience dramatic drops in their blood sugar, causing vision disturbances, headache, fast heartbeat, shakiness, and dizziness; if the low blood sugar is severe and untreated, fainting, seizures, or even a coma can result (via Healthline). Although diabetic ketoacidosis is typically associated with type 1 diabetes, it can also occur in type 2 diabetes if there is prolonged uncontrolled blood sugar or a severe illness or infection, or if someone misses their medication. Diabetic ketoacidosis occurs when the body breaks down fat for energy, and the liver processes the fat into a fuel called ketones, making the blood acidic (via Medline Plus). The body comes to rely on fat because the glucose is stuck in the blood and can't get into the cells.
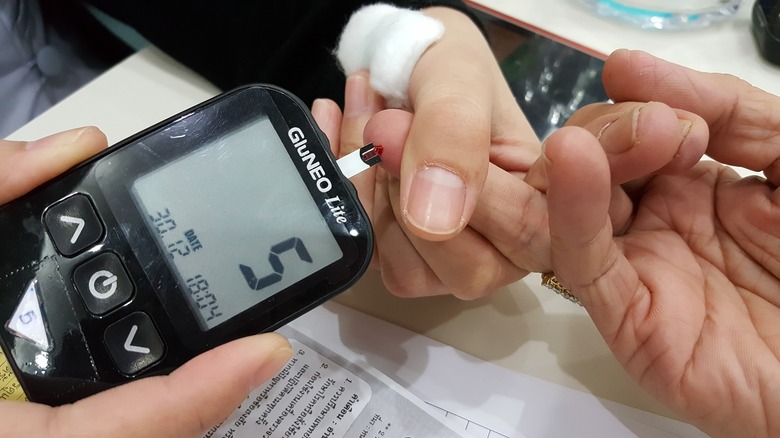
The diagnosis of type 2 diabetes is simple and straightforward
According to the American Diabetes Association (ADA), the A1c test determines what your average blood sugar has been for the past two to three months. You don't need to fast as you do for other tests.
As described by the ADA, diabetes is diagnosed when the A1c is 6.5%, or higher and prediabetes is diagnosed at 5.7% to 6.4%. According to the Centers for Disease Control and Prevention, a fasting blood sugar of 100 to 125 mg/dl indicates prediabetes, and 126 mg/dl or higher is diagnostic for diabetes. This test is usually done after fasting for at least eight hours (via ADA).
Additionally, your doctor may order an oral glucose tolerance test (OGTT), which determines how efficiently your body transports glucose from the blood into the muscle and fat, according to Medline Plus. A sample of blood is taken after you've fasted for eight hours, and then you'll be asked to drink a sugar-containing beverage. Your blood will be taken every 30 to 60 minutes for up to three hours in total to determine how quickly the glucose is removed from your bloodstream and transported into the cells. In individuals other than pregnant women, normal OGTT results are 60 to100 mg/dl fasting, less than 200 mg/dl after one hour, and less than 140 mg/dl after two hours. Between 141 and 200 mg/dl after two hours is considered "impaired fasting glucose," while a result of 200 mg/dl or higher is diagnostic of diabetes.
Oral medications are often the next line of defense after implementing lifestyle strategies
If weight loss, dietary modifications, and exercise don't get blood sugar under control, many doctors turn to oral medications to treat type 2 diabetes. According to the American Diabetes Association (ADA), diabetes pills rarely work for individuals who take more than 20 units of insulin each day or have had diabetes for more than 10 years. However, oral medication will often work for those newly diagnosed and not on insulin.
Sometimes, medication will stop working after a period ranging from months to years, and another medication will be added to it (known as "combination therapy"), the ADA explained. For example, one medication will slow the production of glucose by the liver and the other will decrease the insulin resistance of cells so that more glucose is taken up from the blood (via Pharmacy Today).
As explained by Medical News Today, people with type 2 diabetes and a high risk of complications are given combination therapy immediately, even if their blood glucose is already within the target range. These complications can include chronic kidney disease, having or being at a significant risk for coronary artery disease, or heart failure. The ADA recommends combination therapy if the A1c is 9% or over at the time of diagnosis (via Pharmacy Today).
Injectable medications have made a huge impact on diabetes treatment
In an article for Healthline, Dr. Maria S. Prelipcean, an endocrinologist, explained that there are several types of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) on the market, usually used with other types of treatment that work via different mechanisms.
People with diabetes do not make enough of these hormones, which are normally released by the intestines to increase insulin secretion and bring down blood glucose levels, according to the Association of Diabetes Care & Education Specialists. Therefore, by supplementing with manufactured GLP-1 RAs, glucose levels will be improved and some people lose weight. Importantly, these medications also decrease the risk of strokes and heart attacks.
Endocrinologist M. Regina Castro explained for Mayo Clinic that these drugs help delay the transport of food from the stomach to the small intestine, which help people feel full for a longer time after eating. One of these drugs, liraglutide (Saxenda), is approved to treat obesity in individuals without diabetes. Another non-insulin injectable that is used is amylin analogs. This medication also slows the movement through the stomach, decreasing appetite and preventing blood glucose from getting too high (via Healthgrades).
Sometimes insulin is simply necessary
Clinical Diabetes dispelled some of the pervasive myths about insulin. The publication explained that type 2 diabetes is a progressive disease in which, over time, the pancreas becomes unable to meet the body's need for insulin regardless of how well you've cared for yourself. "If your doctor advises you to start insulin therapy, it doesn't mean you failed to manage diabetes properly," Abbott confirmed. "Diabetes doesn't stay constant."
That's not the only myth some people believe, though. According to Abbott, some erroneously believe that insulin can cause blindness, kidney failure, or death. These are complications of the disease itself, which insulin treats, thereby helping to prevent these complications from occurring. There are many different types of insulin, classified by how long they take to work and peak, how long they are effective for, their concentration, and how they are administered, according to the University of California, San Francisco.
All medications, including diabetes drugs, have side effects
Metformin is by far the most commonly prescribed oral medication for type 2 diabetes (via Everyday Health). According to WebMD, metformin's most common side effects include nausea, gas, bloating, diarrhea, vitamin B12 deficiency, and an upset stomach. Still, these symptoms often lessen over time and are improved by taking the medication with food.
At one time, metformin was believed to cause lactic acidosis. However, the American Diabetes Association clarified that metformin "rarely, if ever, causes lactic acidosis" when used as directed. The increased risk of lactic acidosis "is either zero or so close to zero that it cannot be factored into ordinary clinical decision making." Per Healthline, GLP-1 RAs, on the other hand, decrease appetite and contribute to weight loss (usually in the range of 3.3 to 6.6 pounds). These drugs often cause gastrointestinal side effects, such as nausea, vomiting, and diarrhea, and have been anecdotally linked to pancreatitis. However, it's not clear whether a true relationship exists at this time.
One plus is that GLP-1 RAs are less likely than other types of diabetes treatments to cause hypoglycemia when used alone. According to Drugs.com, insulin's most common side effect is certainly hypoglycemia, which can be serious and even (rarely) fatal. Still, other side effects include blurry vision when insulin is first started, dermatologic reactions (lessened by switching injection sites and maintaining good hygiene), weight gain, and, occasionally, gastrointestinal upset.
The diet for diabetes is not as complicated as people think
As described by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), people with diabetes should eat foods from all major food groups and continue to enjoy all of their favorite foods. However, they may need to choose smaller portions than they are used to eating. Foods that should be limited include fried foods and other foods high in saturated and trans fats, foods high in salt, sweets, baked goods, and beverages with added sugars.
The American Diabetes Association (ADA) recommends counting carbohydrates. Carbs are found in grains, vegetables, fruits, dairy products, beans, sweets, and snack foods. By controlling how many carbohydrates are eaten at meals and snacks, individuals with diabetes can control their blood glucose level. As explained by the ADA, "Because people with type 2 diabetes are resistant to insulin and may not produce enough of it, it's important that you be mindful of your carb intake."
The CDC advises that people with diabetes aim to get half of their calories from carbohydrates. So if you normally eat 1,800 calories a day, that means that you should consume 900 calories from carbs. Since carbohydrates contain 4 calories per gram, that is calculated as 200 to 225 grams of carbohydrates every day. That carbohydrate should be spread evenly throughout the day rather than, for example, eating 100 grams at breakfast, 100 grams at lunch, and 25 grams at dinner. Consistency is key when it comes to planning a healthy diet with diabetes!
Stress management is surprisingly important
When you are stressed, your body releases hormones that increase breathing and blood flow to the muscles and limbs. This triggers a release of glucose, "Your body may not be able to process the glucose released by your firing nerve cells if you have diabetes," Healthline explained. Glucose can then start building up in the bloodstream, thus raising your blood sugar.
The Cleveland Clinic explained that stress can throw off your daily routine and cause wear and tear to the body. Hormones released during the stress response raise blood pressure, heart rate, and blood sugar. When your blood glucose is too low, you might feel blue or tired. When it's too high, some people feel agitated and nervous. You may experience a mix of cognitive, emotional, and physical, and behavioral symptoms, according to HelpGuide. Cognitive symptoms include memory problems and poor judgment; emotional symptoms may include loneliness and isolation or anxiety and agitation; physical symptoms involve frequent colds or flu, loss of sex drive, and diarrhea or constipation; and behavioral symptoms incorporate procrastinating or neglecting responsibilities and nervous habits such as nail-biting and pacing.
Adequate sleep needs to be a priority for individuals who have diabetes
The National Sleep Foundation specifies that one in two people with type 2 diabetes has sleep problems. These sleep problems might be related to high or low blood sugar during the night, stress, depression, or frequent urination. Both restless leg syndrome and sleep apnea are also more common among individuals with diabetes and can profoundly affect sleep quality and duration. The CDC explains that a lack of sleep will increase insulin resistance, increase hunger, make you more inclined to reach for junk foods, and increase insulin resistance, among other things.
Strategies for improving sleep include setting a clear schedule for sleep that you follow every day — not just on weekdays — limiting your exposure to the phone and television for an hour or two before bed, regularly exercising, and practicing relaxation strategies before bed such as reading a book or journaling (via Everyday Health).
What about dietary supplements?
According to the National Center for Complementary and Integrative Health, there is some, albeit weak, evidence to support the benefits of some dietary supplements for diabetics. "For example, chromium might help with blood sugar control, and alpha-lipoic acid might be helpful for diabetic neuropathy (nerve problems)," the NIH detailed. According to the American Diabetes Association, vitamin B12 supplements might be helpful if you have type 2 diabetes and are deficient in the vitamin. People who take metformin for type 2 diabetes have lower vitamin B12 and should consider talking to their doctor about being screened for a B12 deficiency.
An article published in Clinical Diabetes detailed dietary supplements that should be avoided altogether because they can be extremely harmful. These include comfrey, bitter orange, wormwood, kava, and skullcap, among others. Some supplements also pose a particular risk for people taking blood-thinning medications. These supplements include garlic, ginger, ginkgo Biloba, ginseng, and vitamin E.
Additionally, you should be wary of any supplements making bold claims. In September 2021, the FDA issued a warning letter to 10 companies for illegally selling dietary supplements that "claim to cure, treat, mitigate, or prevent diabetes."
Having the right care team can make a world of difference
The American Diabetes Association provides an in-depth list of what providers should be a part of your diabetes care team. A primary care provider can order regular health screenings, treatments for common health conditions, and tests as necessary. Additionally, an endocrinologist, a doctor who specializes in diabetes, will help to fine-tune your treatment regimen. You will also want an ophthalmologist or optometrist to screen and treat you for eye conditions, such as retinopathy, which are more common in those with diabetes, and a podiatrist to regularly check your feet and lower legs for problems that can result from nerve damage caused by diabetes.
You might also want to select a trusted pharmacist to talk to about your medication concerns and potential interactions between medications and supplements. Dental problems are more common among individuals with diabetes, so selecting a dentist is especially important. A registered dietitian, certified diabetes education, and fitness professional can teach you how to avoid complications by planning a healthy diet, manage your diabetes, and develop a safe and effective fitness program. Lastly, a mental health professional can help you deal with the day-to-day challenges of living with diabetes and the more serious emotional issues that might pop up.