Everything We Know About COVID-19 Booster Shots
Over a year after COVID-19 was declared a pandemic, we've come a long way, but the numbers remain worrisome. As of August 20, Johns Hopkins reported that the number of recorded COVID-19 cases around the world had reached 210 million — with over 4 million deaths having been recorded. Close to 5 billion individual vaccine doses have been administered around the world, over a million of which were administered in the immediately preceding eight days, according to the White House COVID-19 Response Team briefing on August 18. However, cases are still rising.
While the FDA-authorized COVID-19 vaccines have proven "remarkably effective," in the words of Surgeon General Vivek H. Murthy, troubling data has emerged indicating that while vaccine protection against severe cases of COVID-19 still remains high, vaccine protection against "mild and moderate cases has decreased over time" (via White House).
The rise in cases is believed to be the result of a combination of decreasing immunity levels and the high transmissibility of the delta variant. Since the data suggest this pattern is more likely to continue than not, the White House announced its plan to offer COVID-19 booster shots to fully vaccinated Americans ages 18 and older, in the hopes of keeping the U.S. "ahead of the virus." Here's everything we know thus far about COVID-19 booster shots.
What is a 'booster' shot?
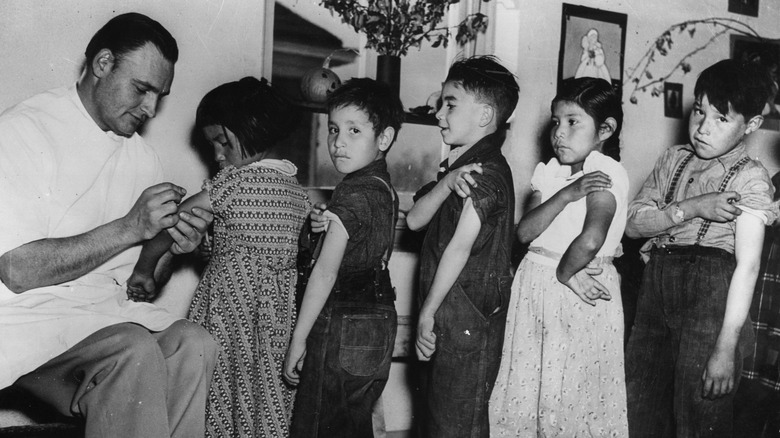
There is a good chance that you have some passing familiarity with the notion of "booster shots." That's because 50 out of 50 states have "school entry requirements for vaccinations," according to the Centers for Disease Control and Prevention (CDC). And many common childhood vaccines require boosters, like the MMR and Tdap (via WebMD). A booster shot is a subsequent shot of the any given vaccine that requires it — at some interval after the original vaccine was given.
Booster shots, like vaccines in general, are part of routine well-health care in the U.S, according to the CDC's Recommended Vaccine Schedule. In fact, sometime in the last 10 years, it's likely your primary care physician or physician's assistant recommended that you get a tetanus booster. Why? Because tetanus can kill you, and in order to remain immune to it, your body needs a booster shot every 10 years (via Healthline).
The bottom line is that some vaccinations require a booster in the form of a subsequent dose of the same vaccine to remain effective as time goes on (via AP News). However, the reason some vaccines decrease in effectiveness over time is considered an unsolved medical mystery at this point (via History of Vaccines). What is known, though, is that unlike the initial vaccine, a booster does not teach your immune system how to respond when faced with the virus in question, but rather, reminds your immune system how to respond.
Why is a COVID-19 booster shot needed?
From even before the COVID-19 vaccine rollout in the United States, scientists in this country and around the world have been following the data as it comes out — both regarding the performance and risks associated with the COVID-19 vaccines authorized by the FDA (via CDC). Thus far, it's been observed that these vaccines are continuing to protect people from severe COVID-19 and death therefrom. However, scientific studies have indicated that the strength of all such vaccines may be waning over time. This leaves the currently fully vaccinated population open to contracting COVID-19 with mild or moderate symptoms. Additionally, the "contagious strength of the widespread Delta variant" increases the need for a booster, explained the August 18 White House press briefing.
This means that an increasing number of vaccinated people may be, or may become, increasingly vulnerable to contracting COVID-19 — many without realizing it due to their mild to moderate symptoms. And they, in turn, can then spread COVID-19 to others, both vaccinated and unvaccinated. In fact, the available data has now made clear this is what's happening.
A number of other countries, including Israel, France, and Germany, are already offering, or planning on offering, booster shots of their existing COVID-19 vaccines (via AP). Other health organizations around the world are moving in that direction. Likewise, the U.S. has concluded that a booster shot will be needed, as it announced on August 18 (via White House).
Is a 'third dose' the same thing as a 'booster shot'?
Prior to the White House announcing plans to roll out COVID-19 booster shots, the CDC had expressed concern about the COVID-19 vaccines potentially not providing the same level of immunity to the immunocompromised population as they do for the general population. This is not strictly a COVID-19-specific phenomenon, but rather something that is seen in the field of vaccinations in general with regard to people with weakened immune systems. Further, data released by the CDC suggest that a large proportion (44%) of "breakthrough" cases of COVID-19 (i.e., cases of COVID-19 that occur after full vaccination) are occurring in immunocompromised people. This is a concern both to such people and also anyone with whom they come into contact.
Accordingly, the CDC has been recommending that people whose immune systems are compromised receive an additional dose of the Pfizer or Moderna COVID-19 vaccine they'd already received. While this might seem like a "booster" shot, the CDC clarified, "This additional dose intended to improve immunocompromised people's response to their initial vaccine series is not the same as a booster dose, given to people when the immune response to a primary vaccine series is likely to have waned over time."
That might sound like splitting hairs, but the point the CDC is making is that discussions regarding booster shots are separate from discussions regarding additional doses for the immunocompromised.
Is the booster shot plan already in place?
According to a joint statement from medical experts and the U.S. Department of Health and Human Services released on August 18, "a booster shot will be needed to maximize vaccine-induced protection and prolong its durability" (via CDC).
"The COVID-19 vaccines authorized in the United States continue to be remarkably effective in reducing risk of severe disease, hospitalization, and death, even against the widely circulating Delta variant," the statement reads. However, due to the nature of the delta variant and decreasing vaccine protection that comes with time, experts advise vaccinated adults to receive a booster shot.
The plan is to begin offering booster shots in fall 2021, although this plan is, as of this writing, "subject to FDA conducting an independent evaluation and determination of the safety and effectiveness of a third dose of the Pfizer and Moderna mRNA vaccines and CDC's Advisory Committee on Immunization Practices (ACIP) issuing booster dose recommendations based on a thorough review of the evidence." Assuming these contingencies fall into place as expected, the Department of Health and Human Services plans to offer booster shots to all fully vaccinated Americans starting on September 20.
How will the COVID-19 booster rollout work?
Booster shots will first be made available to those who were vaccinated earliest, including health care providers, long-term care facility residents, and senior citizens (via CDC). Due to the decreasing vaccine effectiveness that happens with time, this prioritization makes sense. In addition, this plan also takes into account the "continued increased risk that COVID-19 poses to them" as a result of prolonged exposure to the virus and factors such as age and infirmity, per the CDC. Like the initial COVID-19 vaccines, they will be offered free of charge, according to the The Wall Street Journal.
"Our top priority remains staying ahead of the virus and protecting the American people from COVID-19 with safe, effective, and long-lasting vaccines especially in the context of a constantly changing virus and epidemiologic landscape," the joint statement from medical experts and the U.S. Department of Health and Human Services explained.
Those who contributed to the statement include CDC director Dr. Rochelle Walensky; Acting Commissioner of the FDA Dr. Janet Woodcock; U.S. Surgeon General Dr. Vivek Murthy; Director of the National Institutes of Health Dr. Francis Collins; and Chief Medical Advisor to the President Dr. Anthony Fauci. "We will continue to follow the science on a daily basis, and we are prepared to modify this plan should new data emerge that requires it," the experts revealed.
When will you be able to get your booster shot?
According to the joint statement from medical experts and the U.S. Department of Health and Human Services, once booster shots roll out in September, they will likely be offered to all Americans beginning "8 months after an individual's second dose" — albeit with a prioritization schedule similar to the one that applied to the original vaccine rollout except that it will also prioritize anyone else who may have been vaccinated early.
It should be noted, however, that these plans are with regard to those who had either the Pfizer or Moderna mRNA vaccines. "We also anticipate booster shots will likely be needed for people who received the Johnson & Johnson (J&J) vaccine," the statement went on to say. However, in light of the fact that the U.S. did not begin administering the Johnson & Johnson vaccine until March 2021, there is not yet sufficient data to determine the need for a booster. More data is expected in "the next few weeks," revealed the August 18 statement.
"I want to be very clear," said U.S. Surgeon General Vivek Murthy in a White House press briefing the same day, "this plan is pending the FDA conducting an independent evaluation of the safety and effectiveness of a third dose of the Pfizer and Moderna mRNA vaccines and the CDC's Advisory Committee on Immunization Practices issuing booster dose recommendations based on a thorough review of the evidence."
What is the status of the Moderna booster shot?
According to U.S. Surgeon General Vivek Murthy, various analyses have been conducted and are continuing to be conducted regarding the continuing effectiveness of the Moderna vaccine, as well the other FDA-authorized vaccines (via White House). Thus far, the analyses indicate that the Moderna vaccine's effectiveness has, indeed, been declining over time.
The Mayo Clinic's analysis indicated that the Moderna vaccine's effectiveness has declined from 86% to 76% as of July 16 (via White House). This can be considered significant, particularly when considered in light of the fact that the overall effectiveness of all FDA-authorized COVID-19 vaccines has declined to 53% as of August 2021.
The bottom line is that if you received the Moderna vaccine, your body's ability to protect itself when exposed to the coronavirus responsible for COVID-19 may already be declining. This puts you at a greater risk for mild to moderate breakthrough infection with COVID-19, which can also make you contagious to others, including the unvaccinated. Fortunately, Moderna has been testing its booster vaccines in already vaccinated individuals, according to CNBC, which reported that the Moderna booster produces a "promising immune response" against COVID-19 — including the delta variant — and with risks that do not seem to outweigh these benefits.
What is the status of the Pfizer booster shot?
Data from the Mayo Clinic regarding the continuing effectiveness of the Pfizer vaccine may be somewhat more disconcerting than comparable data regarding the Moderna vaccine (via White House). Such data, which was culled with respect to 80,000 vaccinated and unvaccinated individuals, demonstrates that as of July 16 that the Pfizer vaccine's effectiveness against infection declined over time from 76% to 42%. In addition, separate research conducted in Israel shows that the Pfizer vaccine has been becoming less effective at preventing both infection and spread of COVID-19 over time, especially in light of the emergence of the particularly contagious delta variant (via Reuters).
As with the Moderna vaccine, anyone who received the Pfizer vaccine may become more vulnerable to COVID-19 infection over time, putting them at risk for contracting mild to moderate COVID-19 and spreading COVID-19 to others, including those who may be at risk for severe infection. Pfizer has committed to providing the U.S. with 200 million additional doses of its vaccine from October through April 2022, according to The Wall Street Journal. The decision to move ahead with a Pfizer COVID-19 booster shot marks a reversal from the FDA's decision from just a few weeks prior that boosters would not be needed (via NPR).
What about Johnson & Johnson?
The Johnson & Johnson COVID-19 vaccine presents its own unique challenges in terms of getting a booster program rolling. One reason is that the vaccine was not available to the general public in the U.S. until March 2021. In addition, the Johnson & Johnson vaccine is distinguishable from the Moderna and Pfizer vaccines in that it was designed as a one-dose protocol and is not an mRNA vaccine.
However, U.S. Surgeon General Vivek Murthy revealed during the August 18 White House press briefing that he anticipates Johnson & Johnson booster shots, like Moderna and Pfizer booster shots, will become necessary. "We expect more data on J&J in the next few weeks."
As the information comes in regarding the Johnson & Johnson vaccine's continuing effectiveness and the safety and efficacy of a booster, the White House has pledged to keep the general public informed as to whether a J&J booster will be made available and what the terms of its availability will be. Among the questions that the White House and its medical experts hope to answer in the next several weeks and months is whether the Johnson & Johnson booster should be given beginning eight months after initial vaccination (as it is with Moderna and Pfizer boosters).
Should you mix and match?
The prevailing wisdom with regard to mixing and matching COVID-19 vaccines in general has been that individuals should stick with whatever vaccine they have gotten previously for COVID-19 (via NPR). In other words, if your first dose was of the Moderna vaccine, then your subsequent doses should likewise be of the Moderna vaccine. However, this may be changing, according to NPR, which pointed out that using two different vaccines against the same viral threat is not a new concept. It's known as "heterologous vaccination." One example is the polio vaccine, which has been given to children in heterologous form (via Science Direct).
The benefits of heterological vaccination are both scientific and practical. Regarding the latter, remember how in the first few months of the COVID-19 vaccine rollout, you had little to no choice in which vaccine you would receive? Heterological vaccination means that people will be able to get their booster regardless of whether their local vaccine center is offering boosters of the vaccine they received initially. Scientifically speaking, "if you give two different types of vaccine, then you tend to get a better immune response than if you give the same vaccine twice," as immunologist Helen Fletcher told NPR.
Although the CDC has, as of this writing, yet to address choosing a different booster from your original vaccine, they did address mixing and matching third doses among the immunocompromised: "For people who received either Pfizer-BioNTech or Moderna's COVID-19 vaccine series, a third dose of the same mRNA vaccine should be used."
Should you get an mRNA booster if you had the Johnson & Johnson vaccine?
People who received the one-and-done Johnson & Johnson vaccine might be feeling a bit left out of the booster shot zeitgeist right about now, CNBC pointed out. And this may feel quite worrisome with the delta variant running rampant and with so much talk at the moment of the anticipated September booster shot rollout applicable to recipients of the mRNA vaccine recipients (i.e., Moderna and Pfizer). But as Dr. Leana Wen, who teaches public health at George Washington University, pointed out to CNBC, "Patients cannot wait for perfect data," and those whose immune response against COVID-19 is already in decline "need to be given the option."
That being said, Dr. Wen is not recommending that every individual who received the Johnson & Johnson vaccine should now be actively seeking out Moderna or Pfizer booster shots. Although some infectious disease experts are already recommending a booster shot from one of the two approved mRNA vaccines for recipients of the Johnson & Johnson vaccine, it is, in Dr. Wen's opinion, "a complex decision that takes into account your medical history, your family circumstances and who you live with, your COVID-19 exposures, as well as your risk tolerance."
What side effects should be expected with a booster shot?
Something of concern to many is the risk of side effects with booster shots. And as the second doses of the mRNA vaccines were often accompanied by more side effects compared to the first doses, it is something experts are considering. "We're keenly interested in knowing whether or not a third dose may be associated with any higher risk of adverse reactions, particularly some of those more severe — although very rare — side effects," Jay Butler, deputy director at the U.S. Centers for Disease Control and Prevention, revealed during a press briefing (via Reuters). And for recipients of the Johnson & Johnson vaccine, an mRNA booster shot could produce a different set of side effects from what they experienced when they got their initial shot, Dr. Leana Wen, an emergency physician, explained to CNBC.
That being said, more information about the side effects associated with mRNA boosters will become available as more people volunteer to receive booster shots around the world. For example, some countries, including Germany and the U.K., are already giving mRNA boosters to people who received the AstraZeneca vaccine. And, according to CNBC, this protocol appears to be "working well with few side effects." And right here in this country — in San Francisco, California, Johnson & Johnson vaccine recipients are already eligible to request and receive a supplemental dose of one of the two mRNA vaccines.
Rest assured that as more data becomes available, more and more information will become available, too.