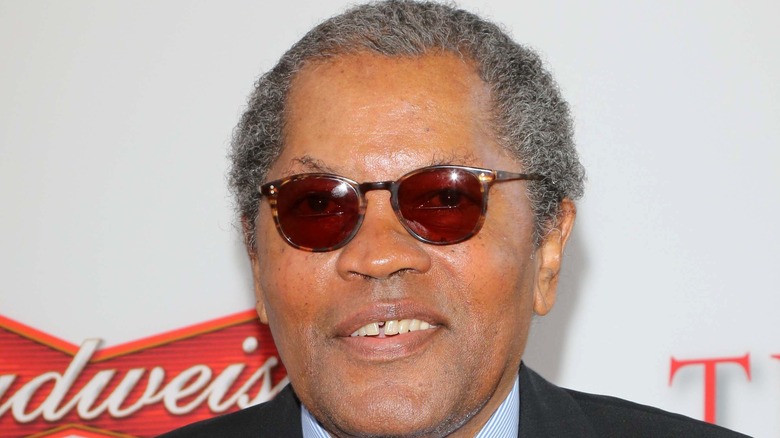
Mod Squad Actor Clarence Williams III's Cause Of Death Explained
Actor Clarence Williams III, who was known for his part in ABC's "The Mod Squad," Dave Chappelle's "Half-Baked," and Prince's father in "Purple Rain," among many other pivotal roles, died at 81.
Williams' management team confirmed he died at his Los Angeles home on Friday after a fight with colon cancer (via the Associated Press). Upon news of his passing, tributes poured out about the inspiration the native New Yorker brought to numerous generations through his work, which spanned from Broadway to hit TV series to feature films over many decades. Williams was one of the first black actors to have a lead role on a TV series (via The New York Times).
He is survived by his daughter Jamey Phillips, and sister, Sondra Pugh. It's not clear how long Williams was battling colon cancer, which is the third most commonly diagnosed cancer in both men and women in the United States (via the American Cancer Society).
What is colon cancer?
Colon cancer typically begins as a growth called a polyp in the large intestine that then becomes cancerous over time. Also called the colon, the large intestine is the final stop in the digestive tract (via Mayo Clinic). This organ is a digestive necessity, as it absorbs water and salt from the remaining food after it goes through the small intestine, then sends leftover waste to the rectum.
There are three types of polyps: adenomas, hyperplastic and inflammatory polyps, and sessile serrated polyps (SSP) and traditional serrated adenomas (TSA). The adenomas, along with the SSP and TSA polyps, are often treated as precancerous (via the American Cancer Society). The hyperplastic and inflammatory polyps are more common and aren't considered pre-cancerous.
Most cancers in the colon and rectum are adenocarcinomas, but there are other rare forms of tumors that can develop. The exact cause of colon cancer remains uncertain, according to the Mayo Clinic.
Symptoms of colon cancer
Polyps are usually small and don't produce many symptoms, making it difficult to identify without regular screening (via the Mayo Clinic). In fact, many people don't experience symptoms in the earliest stages, and when symptoms do appear, they can vary based on the size and location of the polyps.
Some signs to look out for are changes in your bowels like diarrhea, constipation, or narrowing stool lasting more than a few days, along with no relief from a bowel movement. Other symptoms include blood in the stool, cramping or abdominal pain, rectal bleeding, weakness and fatigue, and weight loss (via the American Cancer Society).
It can be tricky to diagnose colon cancer, as many of the symptoms can be caused by hemorrhoids, irritable bowel syndrome, or infection. However, a low red blood cell count can be a telling sign due to blood loss that may have gone unnoticed in your stool. Jaundice or trouble breathing can also indicate signs cancer has spread, according to the American Cancer Society.
Risk factors of colon cancer
There are some lifestyle and genetic factors that can increase the risk of colon cancer. Age is a big factor, as your risk for colon cancer increases the older you get – most people with colon cancer are over 50 (via Mayo Clinic). Your risk for colon cancer also increases if you have a family history of colon cancer, as well as personal history of colorectal cancer, inflammatory intestinal conditions, type 2 diabetes or an inherited gene mutation.
An additional risk factor for colon cancer is based on your ethnic and racial background. According to the American Cancer Society, African Americans have the highest colon and colorectal cancer cases of all racial groups in the United States. Additionally, Jews of Eastern European descent have one of the highest risks worldwide.
Some lifestyle choices are also related to colon cancer risks. Obesity, having a sedentary lifestyle, a low fiber and high-fat diet, moderate to heavy alcohol use, and smoking are some risk factors worth addressing.
Importance of screening for colon cancer
The survival rate of colon cancer is exponentially higher if found at a local stage than if diagnosed early (via the American Cancer Society). For this reason, screening for colon cancer is of utmost importance, and can lead to diagnostic tests if warranted. Colon cancer diagnoses and deaths have been on the slight decline each year (via the National Cancer Institute) – a possible testament to more rigorous screening processes.
There are five tests used for screening if you don't have symptoms – a colonoscopy, DNA stool test, fecal occult blood test, sigmoidoscopy, and virtual colonoscopy. There are risks of false-negatives or false-positives in these screening tests, as well as specific risks to the actual tests themselves, according to the National Cancer Institute.
The American Cancer Society recommends starting screening for colon cancer at age 45, but you should consult with your doctor about specific recommendations and the risks of screening tests.
Treatment options for colon cancer
There are treatment options available for colon cancer, but they are dependent on the stage of the disease and if it has spread throughout the body, as well as your personal health. Stages of colon cancer are 0-4, with 4 being the most serious. Your physician may order an MRI, CT scan, or PET scan to determine your stage (via the National Cancer Institute).
Standard treatment options include chemotherapy, cryosurgery, immunotherapy, radiation therapy, radiofrequency ablation, surgery or targeted therapy. There are additional treatment options being tested in clinical trials, as well as alternative and complementary methods that can be considered.
The American Cancer Society has resources available on cancer information, as well as help getting through cancer treatment. As stated above, it is recommended to speak with a medical professional for advice and to answer any questions you have about colon cancer, its risks, and treatment options.