Popular Medications That Could Reduce Your Risk Of Dying From Cancer
From relying on herbs and plants to manage health and diseases to discovering antibiotics or anesthesia, the evolution of medicine and medications has allowed the human race to live healthier and longer lives. However, when it comes to dealing with cancer, there is still a lot to be learned, and medicinal findings are still happening on a daily basis. Yet, at some point, cancer research shifted from finding and treating tumors to preventing them from developing altogether, seeing that up to 40% of cancers are considered to be preventable (via the National Foundation for Cancer Research). This is where chemoprevention comes in.
Unlike chemotherapy, which kills existing cancer cells, chemoprevention refers to the use of drugs or supplements to reduce the risk of developing cancer in a healthy person, delay its onset when there is a pre-cancerous condition, or prevent its recurrence in someone who's already been treated (primary, secondary, and tertiary prevention, respectively), per OncoLink. Besides preventing cancer, chemopreventive drugs should have two additional characteristics. The first is that they should cause little to no side effects. Nevertheless, this is not always the case, seeing that some drugs may potentially cause anything from hot flashes or a reduced libido to heart attacks or organ failure (via Medical News Today). The second is to be easily accessible, which is why you'll find that some popular medications have been found to serve this purpose. This article tells you more about popular medications you didn't know could reduce your cancer risk.
Understanding off-label drug use
You might be wondering how it is that popular drugs, many of which you probably even have in your own medicine cabinet, can also help prevent cancer. Well, this is thanks to a widely used practice known as off-label drug use. According to the U.S. Food and Drug Administration (FDA), off-label drug use is when doctors prescribe a drug for a purpose, dosage, or route of administration other than what the drug was initially approved for, a practice derived from the necessity to address unmet medical needs, such as when approved treatments are unavailable, ineffective, or unsuitable for either the patient or a specific condition.
In these cases, instead of relying on clinical trials that demonstrate the safety and efficacy of the drug for a secondary condition, doctors rely on their medical expertise in assessing risks versus benefits or on results from research studies that show that the off-label use is also safe and efficient (via Drugs.com). Besides being totally legal, the Agency for Healthcare Research and Quality states that off-label drug prescription is also highly common, with roughly 20% of prescriptions in the U.S. falling into this category. However, the practice does come with some downsides. For example, their cost may not be covered by insurance companies, especially when used for cancer treatments. In addition, as with any medication, the drug might interact with other medicines, cause allergic reactions, or even increase the risk of unwanted side effects (via Drugs.com).
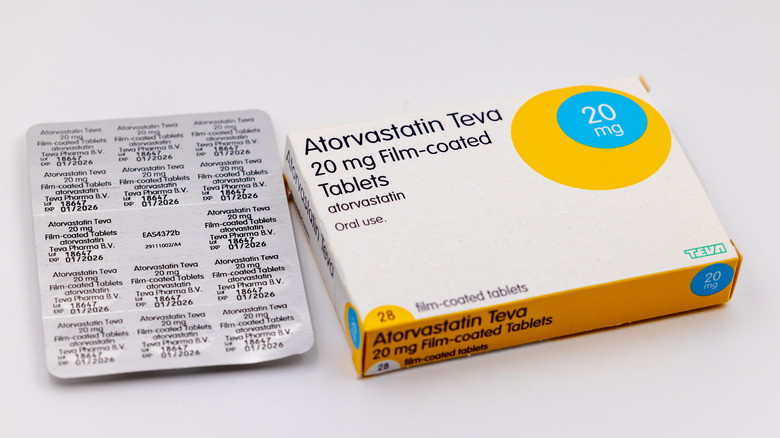
Statins
According to the Cleveland Clinic, statins, such as atorvastatin (Lipitor) or rosuvastatin (Crestor), are a group of drugs prescribed to lower blood cholesterol levels by blocking your liver's internal cholesterol production. In fact, they work not only by reducing LDL (bad) cholesterol but also help reduce triglycerides and may even increase your HLD (good) cholesterol levels, significantly improving markers for heart disease to prevent and manage conditions like heart attacks and strokes. Nevertheless, beyond their cardiovascular benefits, growing evidence suggests that statins may also play a role in reducing the risk of multiple cancers.
For example, according to the National Cancer Institute's Division of Cancer Prevention, due to their anti-inflammatory effect that helps alleviate chronic inflammation (a known risk factor for cancer development), statins might help prevent gynecologic cancers, such as ovarian and endometrial cancers, which happen to have high mortality rates and limited treatment options. Additionally, per a 2018 study in Cancer Management and Research, statin's cholesterol-lowering effects keep cholesterol from reaching cancer cells, which need the fat to grow and multiply, leading to their death (apoptosis). In fact, taking statins for over six months reduced the risk of pancreatic cancer by 67%, while consuming them for more than four years increased the risk reduction up to 80%. According to a 2019 study published in Digestive Diseases, other cancers whose risk seems to become significantly reduced with long-term statin use are gastric, colorectal, and liver cancers. Similarly, a 2023 article in the Journal of the American Medical Association linked statin use to lower breast cancer-related deaths.
Aspirin
Aspirin is a nonsteroidal anti-inflammatory drug (NSAID), meaning that it reduces inflammation without containing steroids, and it is such a widely consumed medication that you can likely find it in every household nationwide. Besides lowering inflammation, aspirin is also effective for pain and fever relief as well as thinning the blood, which is why it is often prescribed to soothe headaches, toothaches, arthritis-related pain, and even for blood clot prevention, a risk factor for heart attacks and stroke (via City of Hope). However, research has made it abundantly clear that aspirin's anti-inflammatory effect may keep chronic inflammation from triggering the development of numerous cancers.
According to the National Cancer Institute (NCI), decades' worth of research has led the U.S. Preventive Services Task Force (USPSTF) to issue a recommendation suggesting that besides lowering the risk of heart disease, long-term aspirin use can also lower the risk of colorectal cancer, the third most common reason people die from cancer in the U.S. (via the NCI). This seems to be because aspirin reduces the formation of new polyps in the colon, a risk factor for this type of cancer (per City of Hope). In fact, studies have linked long-term aspirin use (over six years of intake) with a 19% and 15% risk reduction for colorectal and gastrointestinal cancers, respectively (per the NCI). In addition, according to a 2018 study in Cancer Management and Research, aspirin might also help prevent other cancers, such as pancreatic, esophageal, breast, ovarian, leukemia, endometrial, and prostate cancers. Per the study, aspirin's cancer-preventative effects become more pronounced the longer it is consumed.
Ibuprofen
Ibuprofen is a common over-the-counter medication that also belongs to the NSAID category of drugs. It is sold under brand names such as Advil or Midol to treat menstrual cramps, back pain, and fever for both children and adults (via Drugs.com). As an NSAID, ibuprofen works by blocking cyclooxygenase (COX) enzymes, which are responsible for producing prostaglandins, chemicals in the body that cause pain, swelling, and inflammation (via the Cleveland Clinic). Yet, evidence suggests this anti-inflammatory drug might also hide some anti-cancer properties under its sleeve. In fact, per a 2005 review in Oncology Reports, some studies say that its cancer-fighting effects might even be stronger than aspirins'.
According to a 2020 study in the British Journal of Cancer, it all has to do with ibuprofen's effect on COX enzymes, seeing that by promoting inflammation, these enzymes help create an ideal environment for cancer cells to develop and spread. Thus, by blocking them, ibuprofen hinders their growth. Per the study, long-term ibuprofen intake can lower the risk of colorectal, breast, cervical, gastric, lung, and head and neck cancers. What's more, by inhibiting COX enzymes, ibuprofen also seems to block the development of new blood vessels that support tumors, a process known as angiogenesis, essentially starving cancer cells to death and ultimately slowing cancer's progression (via Healthdor). Lastly, the site adds that some evidence suggests that ibuprofen might also enhance the effects of some chemotherapy drugs, potentiating their cancer-killing properties.
Metformin
While not necessarily a drug that's commonly used by the general population, metformin is a highly prescribed drug for those with type 2 diabetes, as it helps keep blood sugar levels under control. In fact, per the National Cancer Institute's Division of Cancer Prevention, about 40% of people with the condition in the U.S. rely on metformin as a treatment option. According to WebMD, metformin has three mechanisms of action: it slows the absorption of sugar from the digestive tract, reduces the liver's glucose production, and increases the sensitivity of your body's tissues to insulin, allowing sugar to enter the cells instead of remaining in your bloodstream. Still, beyond its intended use, evidence suggests that metformin may also reduce cancer risk.
The National Cancer Institute's Division of Cancer Prevention explains that people with type 2 diabetes have an increased cancer risk because they tend to have both higher inflammation and blood insulin levels, two risk factors for the disease. However, per a 2005 study in the British Medical Journal (BMJ), taking metformin might reduce the risk thanks to its effect on the enzyme AMPK (AMP-activated protein kinase), which is needed for glucose uptake. Since the AMPK enzyme is controlled by a protein called LKB1, its activation also triggers this protein's effects, which also happen to include stopping tumor growth, thus explaining metformin's cancer-fighting properties. Additionally, according to a 2012 review published in Plos One, metformin might also prevent cancer directly by stopping cancer cells from dividing (cell cycle arrest) and triggering them to die naturally (apoptosis) and indirectly by managing body weight.
Antibiotics
Antibiotics are the cornerstone of modern medicine, and they've been highly used ever since their discovery in the 1950s for treating bacterial infections, such as urinary tract infections, pneumonia, or strep throat, significantly reducing complications and mortality (via the Encyclopedia Britannica). They can be classified according to their mechanism of action or their spectrum of activity. For example, the first divides them according to their effect on different bacterial processes, such as cell wall formation or protein synthesis. In contrast, the latter classifies them according to the type of bacteria they target. In any case, they're designed to kill or stop bacterial growth without causing harm to human cells, and emerging research suggests that they may also play a role in reducing cancer risk, namely gastric cancer.
Gastric cancer is among the top 5 most commonly diagnosed cancers worldwide, and one of its most common risk factors is chronic Helicobacter pylori (H. pylori) infections (via the National Library of Medicine). H. pilory is a bacteria that can grow in the stomach lining and survive the stomach's acids, and while the bacteria itself doesn't cause gastric cancer, it promotes the inflammatory environment that allows cancer cells to thrive (per the NCI). However, according to a 2021 study in Biology, antibiotics mixed with probiotics seem to reduce the risk of metachronous gastric cancer. However, the use of antibiotics for cancer prevention comes with risks, such as antibiotic resistance and adverse effects on beneficial bacteria (via MD Anderson Cancer Center).
Tamoxifen
Tamoxifen belongs to a class of drugs known as selective estrogen receptor modulators (SERMs), also known as antiestrogens. As such, SERMs are used to treat conditions that are influenced by estrogen in your body, mainly those seen during the postmenopausal period in people assigned female at birth (AFAB), such as osteoporosis. Yet, some might also help with infertility (via Healthline). Nevertheless, the site explains that tamoxifen is primarily used to treat and prevent estrogen receptor-positive (ER-positive) breast cancer by competing with estrogens for estrogen receptors in breast tissue, blocking their effects and, thus, not allowing the hormone to stimulate breast cancer cell growth.
Besides keeping the cancer from growing in people with this specific type of breast cancer, tamoxifen is also prescribed as a preventive measure for people at high risk of developing breast cancer due to family history or genetic factors (via the Cleveland Clinic). Nevertheless, while this medication is highly effective, it comes with a boxed warning, the most serious safety alert issued by the FDA for prescription medications, seeing as potential side effects include pulmonary embolism, blood clots, and an increased risk of uterine cancer (via Medicine.com).
Proton pump inhibitors
Proton pump inhibitors (PPIs), such as Nexium, are a class of medications primarily used to reduce the production of stomach acid by blocking the action of proton pumps in the stomach lining, which are responsible for producing acid. While stomach acid serves an important function, such as aiding food digestion and killing harmful microorganisms, it may also lead to symptoms such as heartburn. Therefore, PPIs are prescribed to treat conditions like gastroesophageal reflux disease (GERD), stomach ulcers, and Zollinger-Ellison syndrome, as well as to prevent stomach damage caused by chronic NSAID use (via the Cleveland Clinic). Nevertheless, researchers believe that PPIs might also help reduce the risk of certain cancers, especially those associated with chronic acid reflux, such as esophageal cancer, although reports are still mixed.
On the one hand, according to a 2021 review in Translational Cancer Research, Barrett's Esophagus (BE), one of the main complications of GERD, is a risk factor for esophageal cancer. So, by reducing gastric acid and promoting the healing of the esophageal lining, PPIs might reduce the risk of BE progressing toward esophageal cancer. On that note, a study published in Digestive Diseases and Sciences found a 71% esophageal cancer risk reduction in people with BE prescribed with PPIs. In fact, the study mentions that for that reason, up to 98% of people with BE take PPIs, even if they do not have regular reflux symptoms. Yet, on the other hand, per a 2017 review in Plos One, there is not enough evidence to support the use of PPIs for esophageal cancer prevention.
Other ways to reduce your cancer risk
While not all cancers can be prevented, you can still reduce your cancer risk by making some lifestyle adjustments that target modifiable factors that influence cancer development. These factors include your diet, activity levels, body weight, tobacco use, alcohol intake, exposure to radiation, and risk of infection (via the NCI). For starters, following a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding processed foods and limiting red meat and added sugars can help reduce inflammation and lower cancer risk (per the World Cancer Research Fund). Similarly, staying physically active not only protects against cancer on its own but also helps keep a healthy weight, another protective factor since obesity has been linked to numerous cancers (per the NCI).
Moreover, you probably already know that tobacco use has been heavily linked to several cancers, including lung, oral, kidney, stomach, and bladder cancers, to mention a few. Thus, quitting smoking is likely one of the best ways to reduce your cancer risk. On the same note, per Cancer Research UK, reducing your alcohol intake can lower your chances of developing up to seven different types of cancer. Additionally, the site adds that protecting your skin from harmful ultraviolet (UV) radiation through sunscreen, protective clothing, and avoiding tanning beds reduces the risk of skin cancer. Lastly, reducing your risk of viral and bacterial infections, such as human papillomavirus (HPV) and hepatitis B, can lower your chances of developing cervical and liver cancers, respectively (to mention a few), per the NCI. Thus, by making sure you get vaccinated, you'd be taking a proactive step toward cancer prevention.