Unexpected Triggers That Can Instantly Change Your Poop Habits
Despite being an unremarkable and maybe even forgotten part of your day, a healthy bowel movement signals that your digestive system is functioning optimally. However, its balance can be disrupted by unexpected triggers, causing instant and often mysterious changes in your poop habits. Before taking a look into the potential culprits, it's crucial to understand what is known as a normal bowel movement. Since the definition may vary from one person to another, a regular bowel routine is typically characterized by a comfortable passage of well-formed, brown stools with a frequency that goes from thrice a day to thrice a week (per Healthline).
On the flip side, disruptions in your bowel movements can manifest as constipation and diarrhea, acting as red flags indicating that something is amiss within your digestive system. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), constipation manifests as infrequent, hard-to-pass stools, often accompanied by discomfort. Conversely, diarrhea involves loose, runny stools happening more frequently than usual (via NIDDK). Both constipation and diarrhea serve as vital symptoms that help alert you to underlying issues such as stress, infections, or chronic disorders. This article explores some of the potential triggers that can send your digestive system into a tailspin to help you understand how your daily habits, emotions, and health conditions might have the power to alter your poop habits.
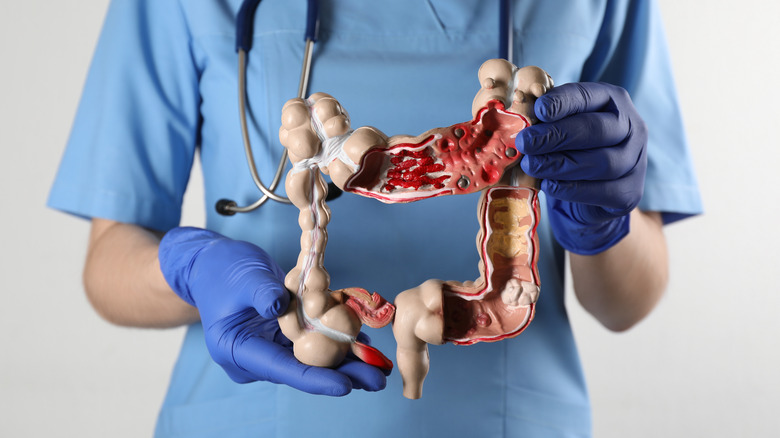
Gastrointestinal disorders
Gastrointestinal (GI) disorders encompass a spectrum of conditions that can significantly impact the normal functioning of the GI tract, leading to alterations in bowel habits and overall digestive health. For example, the Cleveland Clinic lists irritable bowel syndrome (IBS) as a disorder where the intestinal muscles either contract too frequently or seldom do so, creating an irregular muscle activity that can disrupt your normal bowel habits, leading to issues like constipation or diarrhea. On the other hand, conditions like diverticulosis, marked by the presence of small pouches in the large intestine's muscular wall, can lead to constipation-like symptoms when inflamed or infected.
In addition, inflammatory bowel diseases (IBD) like Crohn's disease and ulcerative colitis cause chronic inflammation in the digestive tract, often manifesting with symptoms like diarrhea, which may alternate with periods of constipation (per the Cleveland Clinic). Lastly, celiac disease, an autoimmune condition triggered by gluten ingestion, also causes damage to the small intestine, leading to symptoms that span both chronic diarrhea and constipation, among many others (via Celiac Disease Foundation). Treatment options for these conditions vary depending on the type and severity. Still, many of them have in common the need to adhere to specific dietary guidelines, stress management, and medications to alleviate symptoms and prevent both flare-ups and further intestinal damage. In severe cases, some may require surgical interventions.
Lack of exercise
Exercising is not only beneficial for toning your body or shedding those stubborn extra pounds, but is also a fundamental factor in maintaining digestive well-being, namely preventing and alleviating constipation. The positive impact of exercise on bowel movements is attributed to its ability to fortify abdominal muscles and encourage intestinal contractions, facilitating the fast and smooth movement of stool through the large intestine (via Healthline). According to the Centers for Disease Control and Prevention (CDC), adults should aim for 150 minutes of physical activity per week (preferably the moderate-intensity type), accompanied by at least two days of strength training. These recommendations serve as a blueprint for maintaining overall health, including digestive health.
Per WebMD, even modest efforts like walking for 10 to 15 minutes several times a day can significantly improve constipation symptoms. Beyond walking, a diverse range of exercises, such as running, jogging, swimming, yoga, and dancing, can play a pivotal role in promoting a healthy poop habit. So, the next time you're having a hard time going, think about the last time you exercised and aim to incorporate these activities into your daily life, which will actively contribute to the well-coordinated functioning of your digestive system.
Traveling
It is incredibly common to experience difficulty going number two while traveling, so much so that this phenomenon has its own term: travel or vacation constipation, which can throw a wrench into your trip when you find yourself unable to go according to your usual schedule. As gastroenterologist Dr. Leyla Maric, MD, explains via the Cleveland Clinic, travel constipation can happen after a prolonged flight, road trip, or train journey, primarily due to changes in your routine. Yet, multiple factors may lead to this unfortunate outcome. For starters, a major contributor to travel constipation is inadequate water intake, seeing that dehydration can hinder the movement of waste through your intestines. Additionally, eating unfamiliar foods or drinking more alcohol than usual during your trip can further contribute to this discomfort. Also, travel-induced disruptions to your exercise routine can create a blockage since physical activity has a direct effect on bowel movements by stimulating the muscles of your intestines. Lastly, simply waking up, eating, or going to bed at a different time can mess with your body's internal clock, including your pooping schedule.
The good news is that you can easily combat travel constipation by trying some simple yet effective strategies. Per Healthline, drinking more water, incorporating fiber-rich foods into your diet, staying physically active, responding promptly to the urge to poop, and attempting to maintain your usual sleep, diet, and exercise routine can help alleviate symptoms by restoring the natural flow of your digestive system.
Pregnancy
Pregnancy, a transformative journey for your body, extends its impact to more than just a growing bump by also affecting the functioning of your bowels. According to Healthline, the changes in poop habits during pregnancy are often attributed to hormonal variations and may range from constipation to diarrhea, depending on how far along you are. On the one hand, constipation results from an increase in the hormone progesterone, which is responsible for supporting pregnancy. However, it slows down muscle contractions in the intestines, meaning that your bowels will likely have a harder time moving your stools toward the exit.
On the flip side, the hormone relaxin is released to help your body stretch to accommodate a growing baby, and during the final stages of pregnancy, it helps loosen everything up to prepare your body for delivery. Nevertheless, it comes with one downside, seeing that it may also relax the muscles around your rectum, making it the culprit for loose or watery stools. Yet, while these changes can be disconcerting, keep in mind that these symptoms typically resolve once you give birth. According to the Cleveland Clinic, though you can't prevent the impact of pregnancy hormones on your bowel movements, you can adopt certain measures to ease the discomfort. Incorporating fiber-rich foods into your diet, maintaining adequate hydration, engaging in regular exercise, and discussing the possibility of switching prenatal vitamins with your healthcare provider can all contribute to alleviating symptoms.
Side effects of some supplements and medications
Examining your medicine cabinet could unveil the potential culprit behind your constipation, seeing that certain medications and supplements have been associated with it, highlighting the need to be aware of this undesirable effect. Per GoodRX, the list of drug-related triggers may begin with opioid medications, often prescribed for pain relief, because they may slow down intestinal activity, making regular bowel movement challenging. Similarly, tricyclic antidepressants, which help treat depression and anxiety, pose a risk of constipation by causing the same effect on your bowel movements.
In addition, certain blood pressure, nausea, and overactive bladder medications carry a higher likelihood of causing constipation. Plus, the site explains that antihistamines (allergy medications) and non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve), commonly used for pain and inflammation, can, in some cases, lead to constipation, especially when consumed at higher doses or when taken consistently for an extended period. Lastly, when it comes to mineral supplements, iron takes the lead in this arena, with constipation as a typical side effect. If you suspect a medication or supplement is causing constipation, try consulting with your healthcare provider, as they may suggest adjustments to your medication routine, alternative supportive care measures, or the use of a laxative (per GoodRX). Yet, don't forget that simple lifestyle changes, including increasing your fiber and water intake and physical activity, can play a pivotal role in mitigating constipation, whether it is medication-related or not.
Colon cancer
Colon cancer can manifest with notable changes in your poop habits. In fact, these changes affect about 65% of people with this type of cancer, and they may even serve as a warning sign for the condition, prompting timely medical attention and intervention (via MedicineNet). On the one hand, besides the fact that diarrhea can also be a symptom of colon cancer itself, it is also a prevalent concern for people undergoing cancer treatment, often arising as a side effect of therapies like chemotherapy, immunotherapy, targeted therapy, pelvic radiation, surgical bowel removal, and transplant reactions. In addition, cancer treatments can compromise the immune system, increasing the susceptibility to infections and stomach bugs, which, in turn, may lead to diarrhea (per Cancer Research UK).
On the other hand, while constipation is not a typical bowel movement change associated with colon cancer, advanced stages of colon cancer with tumors large enough to obstruct the colon, a condition referred to as bowel obstruction, may lead to difficulties in passing stools (via MedicineNet). Therefore, managing changes in poop habits related to colon cancer involves a multidimensional approach, and strategies may vary depending on their severity. For starters, it's crucial to see a doctor quickly so they can figure out what's causing the problem and implement appropriate interventions, such as adjusting your schedule and dose of medication or treatment (per Cancer.Net).
Having too much anxiety or stress
Feeling nervous, stressed, or anxious can change your poop habits in a heartbeat, whether by blocking you up or making you run for the nearest toilet. This is because the connection between your emotions (especially stress and anxiety) and changes in poop habits is a direct result of the complex relationship between the brain and the gut, known as the gut-brain axis (via PsychCentral). Stress has the potential to exacerbate stomach issues, including constipation. When you're under stress, your brain triggers the fight or flight response, releasing hormones that redirect blood flow toward the organs that would ensure your survival in a dangerous situation. This means that blood flow to your gut becomes secondary, and as a consequence, digestion slows down, often leading to constipation.
Interestingly, the hormonal cascade induced by stress and anxiety can also have the opposite effect, stimulating muscle contractions in your intestines, which can result in diarrhea or what you may know as nervous poop (via the Cleveland Clinic). Furthermore, according to a study in Expert Review of Gastroenterology & Hepatology, evidence suggests that stress can lead to imbalances in your gut's friendly bacteria, causing issues like inflammation and irregular or slowed-down bowel movements, all of which contribute to changes in bowel habits when stress is prevalent. Managing these stress-related changes in poop habits involves addressing the root cause of stress and employing stress-reducing techniques. Practicing mindfulness, relaxation exercises, and maintaining a healthy lifestyle can positively influence the gut-brain axis, promoting digestive well-being and reducing the impact of stress and anxiety on your poop habits (per PsychCentral).
Neurologic conditions
Several conditions that affect how your brain works can interfere with the messages your brain sends to your gut to let it know when it's time to go number too (and when not to). Such is the case for neurogenic bowel. Neurogenic bowel happens when conditions like spinal cord injuries or nerve diseases (which affect the nerves controlling the lower part of the intestines) cause the loss of normal bowel function. This impairment disrupts the normal storage and elimination of waste, triggering changes in your poop habits that range from constipation to bowel accidents (via Cedars Sinai).
In addition to neurogenic bowel, other brain conditions, such as Alzheimer's disease, Parkinson's disease, and stroke, are associated with changes in bowel habits. According to a study in the Journal of Clinical Investigation, Alzheimer's disease is linked to higher rates of serious gastrointestinal events due to the use of medications like donepezil or rivastigmine, which may induce symptoms like diarrhea. In addition, constipation and fecal incontinence are common symptoms of Parkinson's disease, which may progress with the disease's severity. Lastly, stroke patients commonly experience constipation and reduced rectal sensation, particularly those who have brainstem injuries.
Treatment options for these conditions vary depending on the root cause. Controlling neurogenic bowel involves incorporating scheduled routines for regular stool removal, dietary adjustments, and medications, among other strategies (per Cedars Sinai). As for Alzheimer's disease, the go-to alternative usually centers around changing the dose or type of drugs. Lastly, Parkinson's disease-induced constipation often involves the use of laxatives and prebiotic/probiotic combinations.
Infections
According to Medical News Today (MNT), GI infections include a range of illnesses caused by bacteria, viruses, or parasites, each with the potential to disrupt regular bowel habits and induce symptoms like diarrhea, stomach cramps, vomiting, fever, gas, and bloating (to mention a few). Starting with bacterial infections, these can be attributed to harmful microorganisms (pathogens) like Salmonella or E. coli and are often associated with food-related causes. These infections typically lead to digestive discomfort and are characterized by symptoms such as diarrhea. On the viral front, norovirus stands out as a common culprit, causing what people commonly refer to as the stomach flu. Lastly, parasitic GI infections are caused by intestinal worms or protozoans and include prevalent conditions like giardiasis and cryptosporidiosis (via Healthline).
While parasitic GI infections may call for prescription medications, viral and bacterial infections are typically resolved without specific medical intervention. In fact, hydration plays a pivotal role in self-care for both adults and children dealing with these types of infections, seeing that it helps counteract the effects of diarrhea and vomiting and, thus, prevents dehydration (per MNT). Staying vigilant about hygiene practices is crucial in avoiding GI infections.
Issues with your pelvic floor muscles
The pelvic floor is formed by a crucial group of muscles across the pelvis that support and maintain the proper function of pelvic organs, which include the bladder, urethra, intestines, and rectum (as well as the female reproductive system). When these muscles and connective tissues are weakened or injured, a pelvic floor disorder (PFD) can arise, leading to various complications (via the National Institute of Child Health and Human Development (NICHD)). One such PFD complication is bowel control problems, which typically result in fecal incontinence. Per the NIDDK, fecal incontinence or accidental bowel leakage involves the unintentional passing of poop (which can be either solid or liquid). In other words, this condition may present either as an uncontrollable urge to go or as bowel leakage without awareness.
Treatment options for fecal incontinence can range from simple measures to more advanced interventions (via NIDDK). Basic approaches include diet modifications, over-the-counter medications, bowel training, and exercises aimed at strengthening pelvic floor muscles (e.g., Kegel exercises), which have proven to improve symptoms by approximately 60%. Additionally, other potential treatments include biofeedback therapy, sacral nerve stimulation, non-absorbable bulking agents, and vaginal balloons. Ultimately, if either of these treatments isn't enough, surgery becomes a potential option.
Lactose intolerance
Lactose intolerance is a condition where the body has difficulty digesting lactose, a sugar found in milk and dairy products. As a review in Nutrients explains, a specific enzyme called lactase is needed to break down lactose for absorption in the small intestine. However, after weaning, the activity of lactase decreases as part of a natural process, leading to lactose intolerance. The symptoms of lactose intolerance are diverse and can include abdominal pain, bloating, gas, diarrhea, and occasionally nausea and vomiting (via the Mayo Clinic).
Lactose intolerance-induced diarrhea happens when lactose remains undigested in the colon, causing it to attract water into the intestines, affecting bowel movements and resulting in loose, watery stools. Yet, surprisingly, about 30% of people with lactose intolerance may also experience constipation as a symptom. This happens when methane, a byproduct of flatulence or gas, delays intestinal transit and slows bowel movements. To manage the discomfort associated with lactose intolerance, you can adopt a low-lactose diet. This involves avoiding or minimizing the consumption of dairy products or choosing lactose-free alternatives (per the Mayo Clinic).
Bowel obstruction
A bowel obstruction happens when something blocks the normal flow of stool through the intestines, making it difficult for poop to pass through. Therefore, it is no surprise that constipation is one of its symptoms. In fact, in some cases, it may even lead to obstipation (severe or complete constipation). Other symptoms include abdominal pain, nausea, vomiting, and distension (per the National Library of Medicine (NLM)). According to WebMD, the blockage can be caused by various reasons, such as a physical barrier, a functional issue, or a hardened mass of stool that gets stuck in the digestive tract. The latter, which can be pretty common, is known as fecal impaction, and besides contributing to discomfort, it can disrupt your regular bowel movements.
Per the NLM, the management of bowel obstruction depends on its cause and severity. Stable patients with partial or low-grade obstruction often find relief through nasogastric tube decompression. During this procedure, a thin tube is inserted through the nose and down into the stomach to help remove air, fluids, or other substances and aid with the symptoms. In cases of partial blockages, many resolve spontaneously, aided by dietary changes to ease the strain on the intestines. However, complete or high-grade obstructions may need urgent surgical intervention.
Thyroid dysfunction
The thyroid gland is a crucial regulator of various bodily functions. Thus, it can lead to changes in poop habits when its hormone production is disrupted. According to a study in the World Journal of Gastroenterology, while the mechanisms linking thyroid disorders to GI symptoms are not fully understood, in hyperthyroidism, an excess of thyroid hormones can lead to increased metabolic activity, which affects the gut and results in frequent bowel movements, diarrhea, and even malabsorption with steatorrhea, where fats are inadequately absorbed, resulting in fatty stools. On the flip side, hypothyroidism, characterized by insufficient thyroid hormone production, manifests in decreased metabolic function, impacting the GI tract with sluggish intestinal motility. This often translates to constipation, as the bowel movements become slower.
Nevertheless, you could adopt preventive measures to support thyroid and gut health. The GI Associates and Endoscopy Center suggests trying out strategies that contribute to overall digestive well-being, such as eating more veggies due to their high fiber content, adding probiotics to your diet through fermented foods like yogurt or kefir, including starchy carbs, as well as potassium- and magnesium-rich foods, and staying hydrated with sufficient water intake. Lastly, avoiding foods high in mercury and BPA can also help reduce your chances of triggering an autoimmune reaction or further disturbing your endocrine function.
Laxative overuse
Laxatives are substances designed to help you go number two, and when used appropriately, they play a role in managing constipation. However, laxative overuse can actually lead to dependency, creating the opposite effect (via Healthline). This is because your body learns to rely on laxatives for regular bowel movements. In addition, their long-term misuse can reduce the effectiveness of the usual laxative dose over time, meaning that people end up having to increase their dose for the desired effect (per MNT). One of the main reasons people misuse laxatives is due to misguided attempts to achieve rapid weight loss.
Luckily, laxative overuse can be reversed. To address laxative misuse and dependency, Healthline suggests starting with a gradual reduction in dosage. Simultaneously, maintaining adequate hydration is crucial, seeing that water not only promotes regular bowel movements but also helps soften stools for easier passage. Additionally, eating a fiber-rich diet also helps when you're having trouble pooping, as fiber increases stool bulk and softness. Lastly, staying physically active is another strategy to stimulate bowel function, contributing to a healthier digestive system. Furthermore, per MNT, seeking guidance from healthcare professionals can also provide the support you might need to overcome laxative misuse and restore a balanced and regular digestive function.
When to seek medical care
Changes in poop habits can sometimes indicate underlying issues that require medical attention. Both diarrhea and constipation can lead to complications, and recognizing potential red flags is crucial for seeking timely medical help. According to Stanford Medicine, constipation, while often causing discomfort and irritation, can lead to more serious consequences, such as hemorrhoids, rectal bleeding, and tears around the anus (anal fissures). However, constipation may also lead to severe complications, including rectal prolapse, which is when the large intestine pushes out of the rectum, and fecal impaction. Per the NIDDK, seeking immediate medical attention is essential if, besides having trouble pooping, you notice bleeding from the rectum or bloody stools, abdominal pain that doesn't go away, inability to pass gas, vomiting, fever, or unexplained weight loss.
On the same note, the NIDDK warns that diarrhea, if left unaddressed, can result in complications like mild to severe dehydration and malabsorption, both of which are cause for concern and require prompt medical intervention. When dealing with diarrhea, you should get in touch with your healthcare provider if it lasts more than two days, you have a high fever and frequent vomiting, you count six or more loose stools per day, you have severe abdominal pain, or if stools are black and tarry or contain blood or pus. Additionally, symptoms of dehydration (e.g., dry mouth, dark urine, or dizziness) should not be ignored. Recognizing these red flags and seeking prompt medical help ensures that potential complications are addressed early, leading to better outcomes.