What Is Purpura? Causes, Symptoms, And Treatment
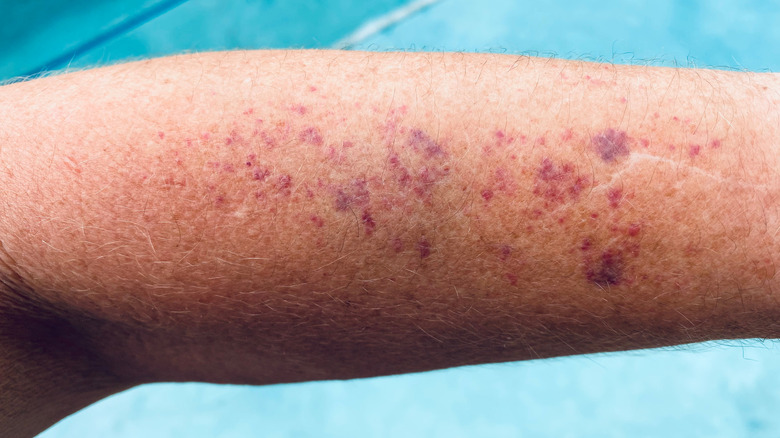
Purpura is a rash in which small spots of blood appear on the skin, notes the Cleveland Clinic. While these flat spots typically occur in a cluster, they can also take the form of an isolated large patch. Purpura can also develop in mucous membranes, including the lining of the mouth and throat. Depending on the skin tone, purpura can appear as reddish-purple or brownish-black spots anywhere on the skin, most frequently on the arms, hands, feet, and legs.
Purpura results from the leakage of small blood vessels beneath the skin surface. It is actually a sign of an underlying condition rather than a medical disorder itself. A variety of underlying conditions lead to a number of different types of purpura. Some types of purpura are associated with low platelet counts caused by several different factors and conditions.
The causes of purpura that is unrelated to platelet levels vary a great deal as well. Risk factors, complications, and treatment of purpura all depend on the underlying condition. It's very important to contact your doctor should you notice signs of purpura (discoloration, blood spots) on your skin. While most cases are not serious, purpura can be caused by severe bleeding resulting from a life-threatening clotting disorder. Here's what you need to know about the condition.
Types of purpura
Purpura is often divided into two major categories: thrombocytopenic purpura and nonthrombocytopenic purpura, reports Medical News Today. Thrombocytopenia is a condition characterized by a low platelet count. Since platelets play an essential role in normal blood clotting, a deficiency of platelets can cause considerable bleeding and bruising. Thrombotic thrombocytopenia (TTP) and immune thrombocytopenia (ITP) are two subtypes of this condition that are associated with abnormal blood clotting and autoimmune-related platelet destruction, respectively.
In other types of purpura, platelets do not play a role. For example, Henoch-Schönlein purpura typically affects children and develops as a result of inflammation in the blood vessels that could potentially cause kidney damage. Solar purpura, also known as actinic or senile purpura, features dark purple or brown patches occurring most often in older age when blood vessels become more fragile. They emerge on the skin as a consequence of long-term sun damage but are also linked to the use of aspirin, anticoagulants, and NSAIDs (nonsteroidal anti-inflammatory drugs).
Some rare versions of purpura are medical emergencies (via the Cleveland Clinic). These are caused by an adverse reaction to anticoagulant medications (e.g., warfarin and heparin) or by a clotting disorder that results in excessive clotting of the blood.
Prevalence of purpura
In the United States, rough estimates of the annual incidence of thrombic thrombocytopenia (TTP) place it at 1.7 million and up to 14.5 per million people, notes MedlinePlus. TTP is more common in women and is far more frequently acquired than inherited.
Immune thrombocytopenic purpura is usually related to an infection or autoimmune disorder (via Immune Thrombocytopenic Purpura). Globally, between 1 and 64 cases of childhood ITP per 100,000 people occur each year, peaking between ages 2 and 5 and again in adolescence. While males have a slightly greater incidence of ITP early on, the incidence in females becomes higher between ages 18 and 45 due to the association of the primary female hormone estrogen with autoimmunity. Children develop ITP more often in the spring and early summer, which are peak times for infections. The annual adult incidence of ITP is 1 to 6 cases per 100,000 people, and increases with advancing age.
Among the types of purpura unrelated to blood clotting, Henoch-Schoenlein purpura occurs primarily in childhood, particularly under the age of 10 and with an annual incidence of up to 20 children per 100,000 (per Henoch-Schoenlein Purpura). The prevalence of actinic, or senile, purpura is about 12% in adults over 50 and increases with cumulative sun exposure (via Medscape).
Signs and symptoms of purpura
According to Medical News Today, purpura generally appears as 4– to 10-millimeter spots on the skin that range in color from purplish red to brownish black and often occur in clusters in a specific area of the body. Purpura can resemble bruises and emerge anywhere on the body, including on mucous membranes inside the mouth.
Some symptoms of purpura require medical attention. For example, due to low platelet levels, some people may experience excessive bleeding in the gums or nose or following an injury. Blood may appear in the urine or stools as well. In other people, purpura may cause fatigue, swollen joints (e.g., ankles, knees), gastrointestinal problems (e.g., nausea, vomiting, diarrhea, abdominal pain), or kidney damage (e.g., protein or blood in the urine).
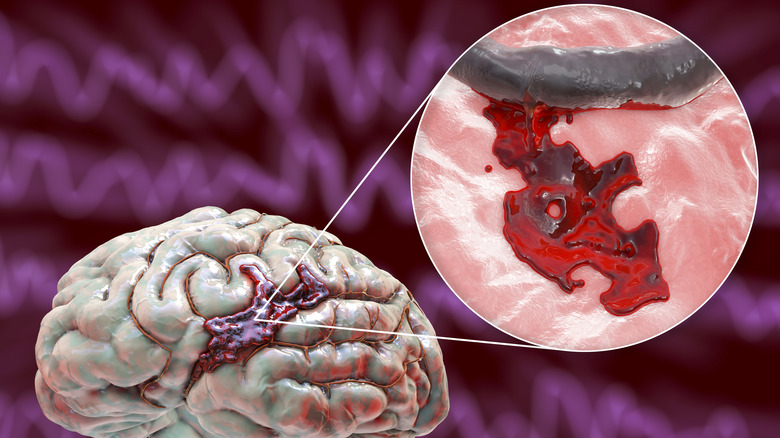
Any trauma to the head is especially concerning in people with immune thrombocytopenic purpura (ITP), per Johns Hopkins. Without sufficient platelets to clot the blood (as in ITP), bleeding in the brain can be fatal. With excessive bleeding, platelet counts can drop below 10,000 — a far cry from the normal number of platelets ranging from 150,000 to 450,000.
Causes of purpura
Thrombocytopenic purpura (platelet-related) is caused by a variety of factors and condition, reports Healthline. For example, some medications can adversely affect platelet function and blood clotting; others may trigger the immune system to produce antibodies against platelets, causing their destruction. People with immune thrombocytopenia as well as lupus also have low platelet counts that are often caused by an autoimmune response. Various infections can also cause low platelet levels, such as viral infections (e.g., HIV, hepatitis C, Ebstein-Barr, rubella, and cytomegalovirus) and tickborne infections (e.g., Rocky Mountain spotted fever). Purpura related to low platelets can even result from a blood transfusion.
Purpura that is unrelated to low platelet counts (nonthrombocytopenic purpura) is caused by multiple factors as well (via Medical News Today). These include infections, allergies, or inflammatory disorders that are associated with abnormal blood production or inflammation of the blood vessels. Amyloidosis is a condition that features the buildup of proteins in the body's organs. Amyloid proteins can also accumulate in the blood vessels of the skin, causing them to become weaker and bruise more easily, notes Stanford Medicine Health Care.
Aging also causes a decline in the structural integrity of blood vessels (per Medical News Today). Other factors that can weaken blood vessels includ inadequate intake of vitamin C and certain drugs (e.g., steroids, sulfonamides).
Risk factors and prevention of purpura
Nonthrombocytopenic purpura that doesn't involve platelet levels is often caused by an underlying condition (risk factor) that is unavoidable (via Medical News Today). Among these risk factors are certain cancers (e.g., leukemia, myeloma), inflammatory disorders (e.g., Ehlers-Danlos syndrome), and infectious diseases, particularly those affecting the very young and old. Other unmodifiable risk factors include advanced age and inherently weak or defective blood vessels. On the other hand, a deficiency of vitamin C can easily be corrected.
With regard to thrombocytopenic purpura (associated with low platelet counts), certain lifestyle risk factors are modifiable, notes Medical News Today. For example, avoiding excessive alcohol consumption, as well as the use of ibuprofen and aspirin, lowers the risk of thrombocytopenia. Platelet counts can be improved by regular consumption of foods rich in vitamin B12, folate, and iron.
Other preventative measures include avoidance of noxious chemicals that can interfere with the production of platelets, e.g., pesticides, benzene, and arsenic.
Diagnosis of purpura
Purpura diagnosis begins with a medical history and skin examination (via the Cleveland Clinic). This will include details such as the size, color and initial appearance of the spots as well as a review of past and current use of drugs and medications. Blood tests and/or a skin biopsy may be ordered by the physician to determine the underlying cause. Blood tests help the physician assess platelet health and potential blood clotting disorders. For example, a complete blood count measures platelets in addition to red blood cells and white blood cells, notes Johns Hopkins. Other tests are used to evaluate bleeding time, rule out infections, and detect antibodies against platelets.
The presence of antiplatelet antibodies may be the cause of low platelet counts. If the antiplatelet antibody test is negative, a sample of liquid bone marrow (where platelets are made) may be analyzed by performing a bone marrow aspiration. This test may be required to determine whether low platelet levels may be due to faulty platelet production or the production of abnormal cells.
A differential diagnosis can help identify causes of purpura related to fragile blood vessels rather than low platelets (via ScienceDirect). For example, the presence of skin atrophy together with purpura may implicate topical steroids while a rounded face, stretch marks, or a hump between the shoulders could point to oral steroid use. While actinic purpura is found only on the hands and forearms, purpura caused by amyloidosis occurs most frequently on the face and eyelids and are very inclined to bleed.
Treatment of pupura
Some mild cases of purpura clear up on their own without the need for treatment, reports Healthline. Aside from those instances, treatment depends on the underlying cause of the purpura. Steroid medications are often used to treat immune thrombocytopenic purpura. By suppressing the immune system, steroids slow the destruction of platelets by antibodies that is characteristic of ITP. However, steroids should not be continued long-term due to potential serious adverse effects such as weight gain, cataracts, and osteoporosis. Intravenous immunoglobulin (IVIG) may be administered when bleeding is severe or as a prep for surgery.
Like steroids, IVIG increases platelet counts but at a faster clip. Newer drugs to treat ITP work by stimulating platelet production in the bone marrow, thereby minimizing bleeding and bruising. These medications include Nplate (romiplostim) and Promacta (eltrombopag). Potential side effects of these drugs include dizziness, vomiting, higher risk of blood clots, and acute respiratory distress syndrome. People with severe ITP who are unresponsive to other treatments may need Rituxan (rituximab), a biologic drug that works by stopping the immune system's destruction of platelets. Low blood pressure, fever, sore throat, and rash are among the potential adverse effects of Rituxan.
In cases of thrombocytopenic purpura that are resistant to any drug treatment, the surgical removal of the spleen (splenectomy) may be recommended. Since most antibody-induced destruction of platelets occurs in the spleen, a splenectomy quickly raises platelet counts. However, it comes with a lifelong increased risk of infection. Extreme bleeding associated with purpura requires emergency transfusions of platelets, steroids, and immunoglobulin.
Natural remedies for purpura
Though conventional drug treatment for immune thrombocytopenic purpura is effective at increasing platelet counts, the downside includes a likely recurrence of the disease, high medical expenses, and considerable side effects (via a 2021 comparative study published in the journal Medicine (Baltimore).
Chinese herbal medicine may provide an alternative therapy for ITP. According to numerous randomized controlled studies, treatment of people with ITP using Chinese herbal medicine has resulted in disease remission, with few side effects. However, different types of Chinese herbal medicine are effective at different stages of the disease, e.g., an acute attack stage, protracted stage, and recovery stage. Accordingly, an ongoing study using meta-analyses has been undertaken to compare various types of Chinese herbal medicine and rank them based on clinical efficacy and safety in the treatment of ITP.
Colchicine, a purified natural product derived from the Colchicum autumnale plant, has been used as a herbal remedy for gout for thousands of years (via a 2018 review of studies published in the British Journal of Dermatology). Studies have demonstrated new therapeutic and preventative applications for colchicine, including the treatment of Henloch-Schonlein purpura in children. Per a 2016 case report in the European Journal of Pediatrics, colchicine was shown to be exceptionally effective, and without side effects, at treating a severe case of pediatric Henloch-Schonlein purpura that did not respond to steroid treatment.
Diet and purpura
A well-balanced, nutritious diet can increase platelet counts and reduce fatigue in people with immune thrombocytopenic purpura (via Healthline). In general, whole unprocessed foods are recommended, including generous amounts of fruits and vegetables, whole grains, fatty fish, skinless poultry, eggs, low-fat dairy, flaxseed, nuts, and nut butters. In particular, two superfoods — avocado and olive oil — are important sources of healthy fats. On the other hand, fast foods, foods and drinks loaded with added sugar (e.g., candy, soda), processed meats (like bacon and pepperoni), and fried foods should be avoided.
Healthful food choices can also mitigate the side effects of medications. For example, limiting consumption of sweets and other simple carbohydrates and eating more calcium rich foods can offset some of the adverse effects of steroid medications (such as high blood sugar, impaired calcium absorption, and increased appetite). Also, to counter nausea from drugs such as Rituxan, a high-protein smoothie may be more appealing and go down easier than a full meal.
Some foods may interfere with ITP therapies. Grapefruit and citrus sodas can block the breakdown of drugs such as the immunosuppressant drug cyclosporin, thus enabling it to remain in the body longer. Excess salt intake is contraindicated for people on steroid medications that may cause fluid and salt retention. Coffee, alcohol, ginkgo biloba, garlic and aspartame may affect platelet function and blood clotting, but only if consumed in huge amounts.
Complications of purpura
The underlying medical condition causing the purpura may lead to complications, notes the Cleveland Clinc. For example, people with immune thrombocytopenic purpura run the risk of bleeding if platelet counts drop below 20,000 (via Immune Thrombocytopenic Purpura).
Bleeding can range from simple skin bruising to gum bleeding to more severe gastrointestinal bleeding. However, brain bleeding is the most critical complication of ITP, usually occurring when platelet counts fall under 10,000. Symptoms of brain bleeding include headache, constant vomiting, confusion, seizures, impairments of nerve/brain function, and/or brain injury. Emergency evaluation and treatment is a matter of life and death.
Henoch-Schönlein purpura, which occurs most often in young children but in adults as well, can also cause complications, reports the Mayo Clinic. Though more common in adults, severe kidney damage may lead to dialysis or even a kidney transplant. A type of rare bowel obstruction may also result from this type of purpura. Known as intussusception, this condition develops when the bowel folds over itself, restricting digestion and blocking the passage of food matter through the gut. Bowel obstruction in children with Henoch-Schönlein purpura can lead bowel ischemia, a life-threatening complication whereby blood flow to the bowel is partially or completely blocked (via a 2020 study published in BMJ Case Reports).
Prognosis
Prompt treatment of the underlying condition (e.g., thrombocytopenic purpura) causing purpura often results in full recovery from the disorder (via Healthline). However, in some people, the purpura spots may not be entirely eliminated and may persist long-term.
Measures can be taken to minimize the development of new purpura spots, though. For example, drugs that lower platelet levels (e.g., ibuprofen, aspirin) should be avoided, as well as high-impact exercise that carries the risk of more bruising or bleeding. Low-impact exercise is less risky and recommended.
Since it usually goes away on its own, the prognosis for Henoch-Söhnlein purpura is excellent, per Medscape. Typically, symptoms disappear within eight weeks; symptoms persist in less than 5% of people with this condition. While some people may experience a recurrence, fatal cases are very rare.
Immune thrombocytopenic purpura can progress to chronic ITP lasting beyond one year in 10-20% children (via StatPearls). Though rare, most deaths from childhood ITP result from infections caused by prolonged therapy with immunosuppressive drugs. In adults with ITP, platelet counts usually stabilize with one or more therapies. Deaths from ITP in adults, though rare, are most often related to bleeding complications. In any case, most deaths in people with ITP are not linked to complications or treatment of ITP.