Babesiosis: What To Know About The Tick-Borne Disease
Parasites are organisms that live in — and feed off of — another organism. Khan Academy explains that the relationship between two organisms can only be considered parasitic if one is gaining something (i.e., the parasite) at the expense of the other (i.e., the host). Otherwise, it is a commensal relationship if one is gaining something but the other is not getting affected by any means; and it is a mutualistic relationship if both parties are benefiting from each other.
Some parasites are completely dependent on the host to survive, while others are only partially reliant. Although most people imagine parasites as tiny little worms, the Centers for Disease Control and Prevention (CDC) explains that parasitic infections in humans can actually be caused by three main types of parasites: helminths, protozoa, and ectoparasites. Helminths are parasitic worms that are often large enough to see with the naked eye. They include flukes, flatworms, and roundworms. On the other hand, protozoa are microorganisms made up of only one cell, which make them too small to be seen without using a microscope. Common examples of diseases caused by protozoa include amebiasis, giardiasis, leishmaniasis, and cryptosporidiosis. Lastly, ectoparasites are a group of arachnids and insects that latch onto the skin and cause disease. These include fleas, lice, mites, and ticks.
Babesiosis is a parasitic infection
Babesiosis is the disease caused by the parasite Babesia. While over a hundred species of Babesia can infect animals, only a handful of them can cause harm in humans. According to Columbia University, the parasite was first discovered infecting animals in the late 1800s, but it wasn't until the mid-1900s in Croatia when experts learned it was able to infect humans as well. Today, cases of babesiosis in humans have been documented in North America, South America, Europe, and even as far as southern and eastern Asia.
WebMD states that cases of babesiosis often arise during the warmer months of the year. In the United States specifically, infection with Babesia has been seen in several states, including Rhode Island, New York, Massachusetts, New Jersey, Connecticut, Delaware, Maine, Minnesota, Wisconsin, and California.
While it is possible for anyone to get infected with Babesia, there are several factors that can increase a person's risk of becoming severely ill. Results from a 2017 study in the American Journal of Tropical Medicine and Hygiene suggest that hospitalization from babesiosis may be more common in adults who are over 75 years old, have underlying heart problems, have no functional spleen, and/or have autoimmune conditions. People who do not receive treatment after a week from exposure, those who have no spleen, or folks with underlying autoimmune diseases may also be more prone to developing severe infection, and may be more likely to require antimicrobial treatment for a longer period of time.
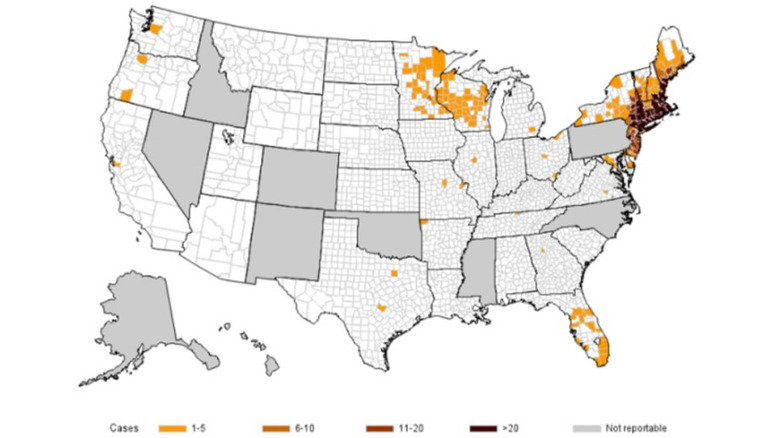
Cases are on the rise in certain parts of the United States
Per a 2017 article in the Journal of Clinical Microbiology, babesiosis has been present in the United States as early as 1968, but epidemiologic data shows that the number of cases has been steadily rising over the past few years. Previously known as the Nantucket fever (following the emergence of several cases in Nantucket Island, Massachusetts in the 1970s), babesiosis has since spread to other parts of the United States, particularly in the Northeast and upper Midwest.
Early in 2023, the CDC published a report indicating that aside from the seven states where babesiosis has already long been established as endemic (i.e., Connecticut, Massachusetts, Minnesota, New Jersey, New York, Rhode Island, and Wisconsin), three additional states (i.e., Maine, New Hampshire, and Vermont) have reported a significantly increased number of cases between 2011 to 2019, prompting the CDC to declare babesiosis as endemic in these three states as well. Alarmingly, the total number of babesiosis cases reported in the United States almost doubled from 2011 to 2019.
Additionally, among the total number of cases reported during the same period, more than 98% of them were from the 10 endemic states, with the top three states with the highest documented cases being New York, Massachusetts, and Connecticut. While it is still unclear exactly why this is happening, the rising number of cases should not be ignored. Thus, it's beneficial to learn about this relatively rare but potentially fatal parasitic infection.
It is infectious but not contagious
Although these two terms are often interchanged, they are actually distinct from one another. GoodRx explains that a disease is described as infectious if it is caused by a pathogen (e.g., bacteria, viruses, fungi, parasites), while a disease is considered contagious if it can spread from one person to another through direct physical contact, touching the same objects, or being in the same room or vicinity as an infected person.
Babesiosis is infectious because it is caused by the parasite Babesia, but it is not contagious because a person acquires it from ticks, not another person. The normal life cycle of Babesia begins when an infected tick bites a mouse and introduces specialized cells called sporozoites into its system. The sporozoites invade the mouse's red blood cells, where it divides into male and female cells. When another tick bites the infected mouse, it ingests both male and female reproductive cells, which eventually unite to form the sporozoites inside the tick's gut. The sporozoites then travel to the tick's salivary gland, where it stays until it can travel to the system of whatever organism the now-infected tick bites next.
Young ticks (i.e., larvae and nymphs) typically latch on to small mammals or birds, while adult ticks attach to large mammals like deer. Incidentally, when an infected tick bites a human being, Babesia sporozoites also invade human red blood cells (causing the signs and symptoms of babesiosis), but their life cycle ends there (per the CDC).
Transmission outside of tick bites is rare but possible
According to the CDC, the primary mechanism of Babesia infection in humans is through a tick bite. In rare instances, babesiosis can be transmitted via blood transfusions, organ transplants, and from an infected mother to their baby through the placenta. Because these latter three modes of transmission do not involve ticks, it can occur throughout the year and in places where babesiosis is not endemic.
Because of a continuous rise in cases of transfusion-related babesiosis, the U.S. Food and Drug Administration (FDA) released a report in 2019, recommending that blood donations coming from Maryland, Virginia, Maine, Massachusetts, Delaware, Minnesota, New Hampshire, Vermont, New York, Connecticut, New Jersey, Pennsylvania, Wisconsin, Rhode Island, and Washington be screened year-round for babesiosis. As for blood donation centers in other states, the FDA recommended that they change their questionnaire to include if they have ever been diagnosed with babesiosis, or had a previous donor screening that indicated they were positive for Babesia.
There are only a few documented cases of transplacental transmission of Babesia (and consequently, congenital babesiosis in the newborn). Reports show that the mothers were either asymptomatic or only had flu-like symptoms during pregnancy. The newborns presented with various signs and symptoms of babesiosis, including hemolytic anemia, low platelet count, jaundice, splenomegaly, and increased bilirubin. They responded well to antimicrobial therapy, with some infants requiring blood transfusions.
Its symptoms can vary greatly
Around a quarter of people with babesiosis will have the disease without experiencing any symptoms, while the rest will have signs and symptoms that can range anywhere between mild to severe. It may take a week to several months before a person develops any signs of infection following exposure to the parasite (i.e., tick bite).
Mild to moderate symptoms of babesiosis are nonspecific, and can include fatigue, weakness, high fever, chills, sweating, loss of appetite (and consequently, unintentional weight loss), headaches, muscle or joint pains, and cough. Without proper treatment, the infection can get worse and lead to severe babesiosis, which can present as yellowing of the skin or white part of the eyes (i.e., jaundice), pale skin, shortness of breath, nausea, vomiting, abdominal pain, dark-colored urine, neck stiffness, and erratic mood swings (i.e., emotional lability). These advanced symptoms are more likely to be seen in older adults, people who are immunocompromised, people who take certain medications, and people with problems with their liver, kidneys, or spleen.
It can be challenging to diagnose
The signs and symptoms of babesiosis are nonspecific, and can be mistaken as something else. However, the suspicion usually becomes high when a person is experiencing the possible clinical manifestations of babesiosis (e.g., fever, flu-like symptoms) and they are living in, or have recently been to, places where the disease is known to be endemic.
If your doctor is suspecting that you may have babesiosis, they will most likely order a simple blood test. Laboratory analysis of your blood may reveal a decreased number of red blood cells, white blood cells, and platelets. You may also have increased lactate dehydrogenase and bilirubin levels, as well as an elevated erythrocyte sedimentation rate (via Columbia University).
All of these results do not necessarily point to a diagnosis of babesiosis, so another test called a peripheral blood smear (PBS) is also often done. People with babesiosis may have visible parasites in the shape of a ring or Maltese cross inside their red blood cells. While this is a very unusual finding, it can also sometimes be seen in people with malaria. Additionally, babesiosis commonly causes destruction of red blood cells, which makes it difficult to visualize the parasites with just one sample. If your blood smears are normal but your doctor is highly suspicious of babesiosis, they may order a polymerase chain reaction (PCR) test to look for the presence of Babesia DNA or an antibody test to see if you have (or had) been infected with Babesia (per Osmosis).
Treatment may include medications and procedures
Medical News Today states that if you have babesiosis but you do not have any symptoms, you most likely will not need any treatment. Likewise, you may not need treatment if your symptoms have resolved before you got diagnosed, provided that no parasites are seen on your peripheral blood smear (via Medscape). However, if you do have symptoms, or if you have any of the risk factors that can increase your risk of developing severe disease, your doctor will most likely prescribe medication.
The American Lyme Disease Foundation (ALDF) states that the first-line medical treatment for babesiosis is a combination of atovaquone (750 milligrams every 12 hours) and azithromycin (500 milligrams once a day on day one, decreased to 250 milligrams thereafter) for 7 to 10 days. Alternatively, you may be prescribed clindamycin (600 milligrams) plus quinine (650 milligrams) every 8 hours for 7 to 10 days. Treatment with clindamycin and quinine can lead to several side effects like abdominal discomfort, ringing in the ears, and vertigo, which is why it is reserved for people who are severely ill or those who do not respond to the first-line treatment. For people who are hospitalized due to severe illness or compromised immune systems, treatment is usually more aggressive and may involve intravenous (IV) medications.
Aside from antimicrobial drugs, patients may also be given fever reducers, medications that increase blood pressure, blood transfusions, hemodialysis, and respiratory support, depending on their disease's severity (via Medical News Today).
It can lead to several complications
Severe, untreated babesiosis can cause a wide range of effects throughout the body. Because Babesia directly invades and destroys red blood cells, it can lead to a condition called hemolytic anemia, where the amount of red blood cells being destroyed outcompetes the body's ability to produce and replace them. Possible signs and symptoms of hemolytic anemia include weakness, dizziness, fever, pale skin, jaundice, heart murmurs, and an enlarged liver and/or spleen. Consequently, an enlarged spleen can rupture, resulting in a medical emergency with additional symptoms of upper left abdominal pain and tenderness, left shoulder pain, and lightheadedness. Splenic rupture can cause significant and fatal bleeding if it is not addressed immediately.
Per Cleveland Clinic, other possible complications of babesiosis include fluid buildup in the lungs (i.e., pulmonary edema), disseminated intravascular coagulation (DIC), and organ failure. Pulmonary edema can initially present as difficulty breathing, but it may eventually result in heart failure or respiratory failure. DIC is a condition where the body's clotting system becomes overactive. Paradoxically, platelets get consumed, which ultimately leads to uncontrollable bleeding. In people who are at high risk of infection (especially those without a functioning spleen), multiorgan failure is common, especially involving the kidneys and liver (via StatPearls). These complications can result in death if not managed closely in the hospital. Unfortunately, while most people are expected to fully recover from a Babesia infection, it is estimated that death occurs in around 10% of people who are hospitalized for babesiosis.
There are ways to reduce your risk of getting it
One of the best ways to protect yourself from babesiosis is by avoiding places known to have ticks. If this is not possible, there are other ways you can lower your risk. When not attached to hosts, ticks are often found on overgrown grasses and piles of leaves. Protect yourself by walking on clear paths and watching your surroundings. Ticks are also more likely to latch on to your skin if they are exposed. To get ahead of this, wear long-sleeved tops, long pants, socks, and closed shoes when walking outdoors. Pull your socks over your pants to prevent ticks from crawling up your legs. Additionally, if you wear lighter-colored clothes, it will be easier to see if there are ticks on you.
You can also spray tick repellents directly onto your skin or all over your clothes, just make sure that it contains DEET. Depending on the product, you may need to reapply it after a few hours. There are also products that contain permethrin, a medication used to kill lice and mites. These are applied to clothing and shoes, but should not be applied to your skin (per the CDC).
Check your whole body for ticks regularly right before you go back indoors. If you have a pet, check their skin thoroughly as well. If you see a tick, grab it by its mouth parts using tweezers and gently pull straight, away from the skin (via WebMD).
It has some similarities with Lyme disease
Lyme disease is a bacterial infection caused by Borrelia burgdorferi, and is transmitted through a bite from an infected tick, the same kind of tick that can transmit babesiosis. Studies show that ticks can become co-infected with more than one pathogen, including those that cause babesiosis and Lyme disease (via the National Institute of Allergy and Infectious Diseases). Research on mice also revealed that those who were bitten by co-infected ticks (with at least one infection coming from Borrelia) developed a more severe form of Lyme disease compared to those who were bitten by ticks with only one infection. As cases of tick-borne illnesses have been increasing (per NBC News), we should be aware of the possibility of getting infected by more than one pathogen at the same time.
Lyme disease can be categorized into three stages. The first stage begins days to weeks following a tick bite. A unique "bulls-eye" rash appears, accompanied by nonspecific symptoms like fatigue, muscle aches, appetite loss, and fever. Weeks to months afterward, the infection spreads to other body areas, initiating the second stage. More "bulls-eye" rashes may appear, and you may experience migrating body pain, headaches, neck stiffness, numbness and tingling, shortness of breath, and palpitations. Months to years later, you may start to experience nerve, sleep, and mood problems, which usually means that you have progressed to the third stage (per Harvard). Although it is associated with several signs and symptoms, Lyme disease is curable with proper treatment and is rarely ever fatal (via Cleveland Clinic).
It should not be confused with malaria
Babesiosis is commonly confused with malaria because the parasites that cause them can be difficult to distinguish (even microscopically) from one another. Babesiosis is caused by Babesia, while malaria is caused by Plasmodium. However, unlike babesiosis, malaria is transmitted through a mosquito bite. It can also be transmitted from one person to another via blood transfusions, through the placenta, and by sharing injection needles (per Mayo Clinic).
The clinical manifestation of malaria is somewhat similar to babesiosis, with symptoms including fever, fatigue, muscle aches, abdominal problems, dark-colored urine, spleen enlargement, and liver enlargement. Severe malaria infections can also lead to hemolytic anemia, DIC, organ failure, and death (via the CDC). But compared to babesiosis, malaria is more well-known throughout the world, and is recognized for its tendency to cause serious disease especially in Africa and Asia. In the United States, reported cases of malaria are often from people who recently came from (or traveled to) endemic areas (per the CDC).
According to the World Health Organization (WHO), the number of malaria cases and deaths throughout the world increased during the COVID-19 pandemic, with the majority of cases still occurring in the region of Africa. Treatment of malaria depends on what species of Plasmodium is causing the infection, drug resistance, the age of the person being treated, and whether the infected person is pregnant or not. Malaria can be prevented by avoiding mosquito bites, staying away from endemic areas, and sometimes taking preventive medicines.