Lipitor Explained: Usage, Dosage, And Side Effects
Heart disease is a term used to group a range of chronic conditions that affect the heart and blood vessels, including coronary artery disease (CAD), heart attacks, heart failure, and irregular heartbeat. According to the Centers for Disease Control and Prevention (CDC), it is the leading cause of death in the United States, affecting people regardless of their gender, race, or ethnicity. Therefore, heart disease is considered a significant public health concern that results in astronomical financial costs not only to those who live with it but to healthcare providers, and to employers as well, considering the cost of prescription medications and productivity loss.
Some of the risk factors that can increase a person's likelihood of developing heart disease include age, family history, smoking, excess weight, leading a sedentary lifestyle, consuming too much alcohol, following a diet high in saturated and trans fats, salt, and sugar, and having high cholesterol levels. Luckily, drugs such as Lipitor help you manage your blood cholesterol and triglyceride levels to help to reduce the risk of heart disease. Lipitor (atorvastatin) is part of a class of drugs known as statins, which work by reducing the production of cholesterol in the liver. This article tells you all about Lipitor and what makes it different from other available treatments.
What are cholesterol and triglycerides?
Have you ever heard that cholesterol and triglycerides are bad for your heart health? Well, this is only partially true. Cholesterol and triglycerides are two types of fats that flow freely in the bloodstream and play important roles in the body. According to a review published in the journal Frontiers in Bioscience-Landmark, cholesterol is an important element of cellular membranes needed for signaling purposes. It also helps produce hormones such as vitamin D or the sex hormones estrogen, testosterone, and progesterone. Furthermore, your body needs it to create bile acids, which help with the digestion of dietary fats and manage the metabolism of sugars. Also, there are two types of molecules that carry cholesterol throughout your body, and they're not all bad. Per the American Heart Association (AHA), low-density lipoprotein (LDL) cholesterol is the "bad" kind that contributes to heart disease. In contrast, high-density lipoprotein (HDL) cholesterol is the "good" kind, which protects against heart disease.
As for triglycerides, another review published in the journal Comprehensive Physiology explains that triglycerides are not only designed to help store excess energy from foods, but they help transport said energy to other tissues and cells. Per the AHA, both cholesterol and triglycerides are produced by the liver, yet they are highly influenced by factors such as diet, exercise, and genetics. For example, since animals also have livers that produce their own cholesterol, a diet rich in animal-based foods contributes to your total cholesterol levels. Similarly, processed foods with a high content of saturated and trans fats also add to the cholesterol produced by your liver, which may cause it to rise above normal levels.
The consequences of high cholesterol
According to the AHA, having high blood cholesterol levels can lead to a number of serious health problems, including atherosclerosis, heart attacks, stroke, high blood pressure, and peripheral artery disease (PAD). Per the CDC, atherosclerosis is when your arteries become clogged by a buildup of plaque, a cholesterol-based substance that narrows the inside of your arteries, making it difficult (or sometimes impossible) for blood to flow freely, which means that the blood supply to your organs or tissues slows or stops.
For example, if the arteries that supply blood to your heart become clogged, you may experience a heart attack, but if it happens to the blood vessels that deliver blood to the brain, you may experience a type of stroke, the CDC explains. Similarly, if the arteries that carry blood all the way down to your legs (also known as peripheral arteries) become clogged, you may experience PAD. Lastly, when cholesterol causes the inside of your arteries to become narrower than they should be, your body works harder in an attempt to try to maintain blood flow, which leads to an increase in blood pressure.
How does Lipitor work?
Lipitor (atorvastatin) is a commonly prescribed medication for managing high blood cholesterol levels that belongs to a group of drugs known as statins, or HMG-CoA reductase inhibitors. According to Statin Medications, said drugs help lower total blood cholesterol levels, as well as low-density lipoprotein (LDL) "bad" cholesterol and triglycerides, yet also help increase high-density lipoprotein (HDL) "good" cholesterol levels. Statins work by blocking an enzyme called HMG-CoA reductase, which is responsible for cholesterol synthesis in the liver. Thus, by reducing your body's own cholesterol production, Lipitor keeps cholesterol from building up in the walls of arteries and reduces the risk of heart disease and stroke (via Drugs.com).
Furthermore, Statin drugs can be grouped or categorized based on their potency in lowering LDL (bad) cholesterol levels. High-intensity statins such as Lipitor 40 mg and Lipitor 80 mg are estimated to generate a 50% reduction in LDL (bad) cholesterol levels. These types of statins are prescribed for people with dangerously high blood cholesterol levels. In contrast, moderate-intensity statins, like Lipitor 10 mg, are expected to reduce LDL (bad) cholesterol levels by 30–49%, and other statin drugs classed as low-intensity statins are believed to generate a reduction of less than 30%. According to the brand's website, you can expect the effects of Lipitor to start working after two weeks of taking the medication.
How to take Lipitor
Lipitor comes in tablet form. It is available in four strengths (10, 20, 40, and 80 mg), which you can easily find marked on one side of each pill. Per the medication's instructions, Lipitor is taken once a day, and while it can be taken with or without food, you should try to take it at the same time each day. If you miss or forget a dose and it has been less than 12 hours since your regular Lipitor schedule, you should take it as soon as possible. However, if you're closer in time to the next dose, the brand suggests skipping the missed dose and just continuing with the following one. Whatever you do, do not take two doses together (via Lipitor).
Also, since Lipitor tablets are film-coated, the drug's instructions state that you should avoid breaking them before taking them. This is because film-coating may help control the drug's release time or properties, or protect sensitive ingredients (per Pharma Central). Furthermore, you should already be following a low-fat diet before taking Lipitor. Regarding dosage, it will depend on your blood cholesterol levels. However, your doctor may increase or decrease it as needed. Typically, adults may start with 10 or 20 mg per day and increase to a maximum of 80 mg daily, while children over 10 years old usually begin with a 10-mg dose, and the maximum can vary between 20 mg and 80 mg depending on each case (via the Mayo Clinic). Lipitor is not approved for children under 10 years old (per Lipitor).
Lipitor may interact with other drugs or foods
Lipitor can interact with other drugs and certain foods, which may alter its effectiveness or increase the risk of side effects. Per Drugs.com, Lipitor actually interacts with 346 different drugs, of which 13% are considered major interactions that could have a significant clinical impact (meaning that the risk of combination outweighs the benefits of taking the drugs), 77% are considered moderate interactions, which should only be used under special circumstances as prescribed by a medical professional, and 10% are deemed minor interactions, which means that they are minimal and have little clinical significance. Some common drug interactions with Lipitor include antifungal drugs, antibiotics, birth control pills, protease inhibitors, and other heart medications (via Statin Medications).
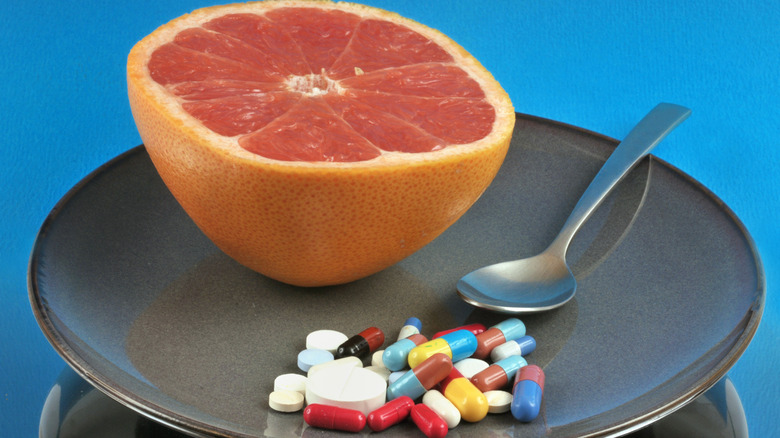
Furthermore, Drugs.com warns that mixing Lipitor with alcohol may increase the risk of liver damage. The site also explains that consuming citrus fruits like grapefruit, lime, pomegranate, pomelo, and Seville oranges with Lipitor should be avoided due to the citrus' furanocoumarins content. In nature, furanocoumarins help protect fruits from insects and infections. However, furanocoumarins such as bergamottin are known for being powerful statin-interacting substances that may cause a spike in statin levels, increasing the risk of more serious side effects. Of all citrus fruits, grapefruits and their juice have the strongest interaction with Lipitor and, thus, should be thoroughly avoided.
Potential side effects of taking Lipitor
Like all medications, Lipitor can cause side effects. Some of the most common ones include muscle and liver problems. According to Medical News Today, muscle pain, weakness, or tenderness are experienced by up to 29% of people who take statins. In fact, these side effects are so common that they are often referred to as statin-associated muscle symptoms, or SAMS. While the cause is not yet entirely understood, SAMS are usually mild and go away after stopping or lowering the medication's dose. Nevertheless, though rare, higher doses have been linked with rhabdomyolysis (or rhabdo), a condition where skeletal muscle breaks down rapidly (per Lipitor). As for liver problems, Lipitor has been linked with liver-related symptoms such as tiredness, appetite loss, upper belly pain, dark-colored urine, and your skin or the whites of your eyes turning yellow. Be sure to contact your healthcare provider immediately if you notice any of them.
Other side effects of taking Lipitor may include nausea and vomiting, upset stomach, diarrhea, and skin and allergic reactions, such as swelling of the lips, face, tongue, or throat, which are considered severe and require immediate treatment due to the possibility of blocking the airway and causing difficulty breathing. Also, people with diabetes may experience high blood sugar levels when taking statin drugs. Lastly, some less common side effects of the medication seen in clinical studies include memory loss, confusion, tendon problems, joint pain, and urinary tract infections.
Some people should avoid taking Lipitor
According to the drug's safety indications, people with active liver disease are advised to avoid taking Lipitor. This is because the liver is responsible for metabolizing the drug and removing it from the body, and a diseased liver may not be able to effectively do so, leading to potential increases in liver enzymes. However, a review published in the journal Current Treatment Options in Cardiovascular Medicine states that this might only be true for people with decompensated cirrhosis and acute liver failure who may not benefit from taking statins. Yet it may not be the case for people with chronic liver disease, such as Non-alcoholic Fatty Liver Disease (NAFLD), stable or compensated cirrhosis, and hepatitis C virus, who generally tolerate statins.
In general, people with liver disease are advised to use medications with caution. Thus, it is vital to inform your doctor about your medical history, including any liver problems, before starting Lipitor (or any other drug, for that matter). Your doctor may order liver function tests before and during treatment with Lipitor to monitor liver function and ensure that the liver is able to tolerate the drug. In addition, people with hypersensitivity or allergies to any of Lipitor's components should steer clear from taking this specific cholesterol-lowering drug.
Lipitor for pregnant and breastfeeding people
In general, pregnant and breastfeeding people are advised to use medications only when the potential benefits outweigh the potential risks, and to avoid medications that are not known to be safe for the fetus or nursing babies. In the case of Lipitor, it is not recommended for use during pregnancy and breastfeeding because its safety has not been established in these populations (via Lipitor). As the drug's safety information card explains, since Lipitor reduces the body's internal cholesterol production (and potentially the levels of other biologically active substances derived from cholesterol as well), taking Lipitor during pregnancy may harm the fetus, and there is not enough available evidence to confirm or discard the risk of congenital malformations or miscarriage. Thus, its intake should be discontinued as soon as you suspect or confirm a pregnancy. If you are pregnant and have high cholesterol levels, your doctor may recommend lifestyle changes such as a balanced diet and regular physical activity to help manage your cholesterol levels.
As for its use in breastfeeding people, Lipitor is also contraindicated during this time because it has not yet been determined whether the drug can be passed on to the baby through breastmilk (other statin drugs are known to pass into human milk, and animal studies show that Lipitor can pass into rat milk). If you are breastfeeding and have high cholesterol levels, your doctor may recommend switching breastfeeding for infant formula so you can continue taking Lipitor (via Healthline). Your doctor can help you determine the best course of action for your individual situation.
How much does Lipitor cost?
The cost of Lipitor can vary depending on multiple factors, including the strength of the medication, the pharmacy where it is purchased, and whether or not it is covered by insurance. For example, a 90-day supply of Lipitor may go from $1,178.89 for the 10-mg dose (or $13.10 per unit) to $1,677.61 for the 80-mg pills (or $18.64 per unit) for people who pay in cash and don't have insurance (per Drugs.com). However, there are various assistance programs available that offer better purchase prices and options, including the Lipitor savings card, copay programs, and rebates.
The Lipitor savings card offers eligible people a deal of $4 for each 30-day supply. You might qualify for this card if you don't have an insurance plan, your insurance is directly purchased by you or your employer, or your insurance isn't a state or federal healthcare program like Medicare or Medicaid (via Lipitor). Lipitor's savings card is valid at participating pharmacies only. Nevertheless, you can also ask for reimbursement when purchasing Lipitor at nonparticipating pharmacies or through mail-order pharmacies.
Crestor versus Lipitor
Lipitor (atorvastatin) and Crestor (rosuvastatin) are medications used to treat high blood cholesterol levels. They both belong to a class of drugs called statins, which work by blocking the liver's cholesterol production and are effective at reducing low-density lipoprotein (LDL) "bad" cholesterol to reduce the risk of heart disease and stroke (per Drugs.com). Since they belong to the same group of drugs, Lipitor and Crestor share a couple of similarities, including their cholesterol-lowering effects and overall indications on how to take them.
Nevertheless, they also have a couple of differences. For starters, both drugs share some potential side effects, such as muscle pain, nausea, diarrhea, and headache. However, some side effects that are exclusive to Crestor include depression, nightmares, and trouble sleeping. In contrast, side effects exclusive to Lipitor include gas and fatigue (via RxList). Also, grapefruit and its derived products don't interact with Crestor the way they do with Lipitor, meaning that you can consume them without risk. Lastly, Crestor is a more economical option for people who don't have insurance or don't qualify for assistance programs (per Drugs.com).
Repatha versus Lipitor
While both Lipitor and Repatha (evolocumab) are medications used to lower blood cholesterol levels, they belong to different classes of drugs and have different mechanisms of action (via Drugs.com). Lipitor is a statin that works by stopping cholesterol production in the liver. In contrast, Repatha is a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor, which works by blocking the PCSK9 enzyme and allows for low-density lipoprotein (LDL) "bad" cholesterol to be removed from the bloodstream (per Drugs.com).
Additional differences between the two include their forms of administration, with Lipitor being a pill that's taken orally, while Repatha is an injection given under the skin. Furthermore, Lipitor must be taken on a daily basis, whereas Repatha is usually taken every two to four weeks. Moreover, Repatha is associated with a lower risk of muscle-related side effects than Lipitor, but may be linked to a higher risk of other side effects, such as skin reactions at the injection site, allergic reactions, and flu-like symptoms (via Drugs.com).
Alternatives to Lipitor
There are numerous reasons why you may not qualify for or choose not to take Lipitor. Luckily, there are other therapy alternatives to consider. On the one hand, some additional prescription drug options include bile acid sequestrants, cholesterol absorption inhibitors, and fibrates. Bile acid sequestrants keep bile acid from being absorbed, meaning that your liver must turn to cholesterol to produce it, thus lowering your total blood cholesterol levels (via Medline Plus). In contrast, cholesterol absorption inhibitors block the intestinal absorption of cholesterol from foods, which keeps your cholesterol levels from rising (per Drugs.com), while fibrates reduce your triglycerides levels (via the Cleveland Clinic).
Still, keep in mind that all of these alternative medications are prescription drugs and should only be used under the supervision of a healthcare provider, as they may have different side effects and drug interactions and may not be appropriate for everyone. Moreover, remember that exercise and dietary changes are key elements for improving heart health. These lifestyle changes can help reduce cholesterol levels, even if medication is also needed. According to the AHA, eating a heart-healthy diet rich in legumes, whole grains, fruits, vegetables, white meats, and nuts, while being low in red and processed meats and sugars is the best way to manage your cholesterol levels, as well as engaging in at least 150 minutes of physical activity per week.