In Vivo Versus In Vitro: What's The Difference?
Having a baby can be an exciting experience to look forward to, but when it comes to fertility treatments things might begin to become confusing amid the medical jargon and array of options to help you grow your family. The New York Times reports that since the year 2010, there have been monumental advances in science and technology when it comes to fertility treatments. The success of freezing eggs and ovarian tissue has risen drastically, approaches to overcoming male infertility have been developed, and surgeries to preserve fertility in patients with cancer have become more refined. As fertility treatments continue to progress in effectiveness, you're likely to hear many terms, jargon, and acronyms in the mix.
One of the most common acronyms in the world of fertility treatments is IVF, which stands for in vitro fertilization (via MedicalNewsToday). Not to make things more confusing, but there is also a technique called in vivo, which shares similarities and differences with in vitro fertilization treatments. The Latin roots of the names of these processes can clarify the distinction between in vivo and in vitro, with in vivo meaning something that takes place in a living space and in vitro referring to taking place in glass. The etymology of these treatment names may offer an indication of how each fertility treatment is conducted, but there's a lot more to know when it comes to learning about the differences between in vivo and in vitro, as well as which option may be right for you.
In vivo technology is newer
Simply put, in vivo fertilization refers to the meeting of a sperm and an egg inside of a living being, according to Healthline. The term in vivo can also be used to reference any form of internal process within a living being, such as animals. In the case of human fertility, in vivo generally implies egg fertilization that occurs inside a woman's body.
Traditionally, in vivo fertilization has referred to natural conception that occurs when sperm is inserted into a woman's reproductive system, but the technology to create successful embryos via in vivo methods without the component of sexual intercourse is currently being pioneered (via Nova IVF Fertility). There are technological advances for in vivo conception and development of embryos inside of a woman's womb that have been successfully performed in recent years, per IVI Bilbao. The mechanism of newfound techniques for in vivo fertilization focuses on inserting tiny capsules, which are smaller than a single millimeter, containing embryos and thousands of microscope holes within the capsules to allow the embryos to attach for proper development.
The drawback to in vivo technology is that because it is so new, it isn't widely available at present.
In vitro is more common than you may think
In contrast to in vivo technology that is only just emerging, in vitro fertilization (IVF) has been around for years and has become a common fertility treatment. The popularity of IVF has reached new heights and now annually results in the births of approximately 4 million babies in the United States, thus accounting for up to 2% of births nationwide, as reported by Penn Medicine.
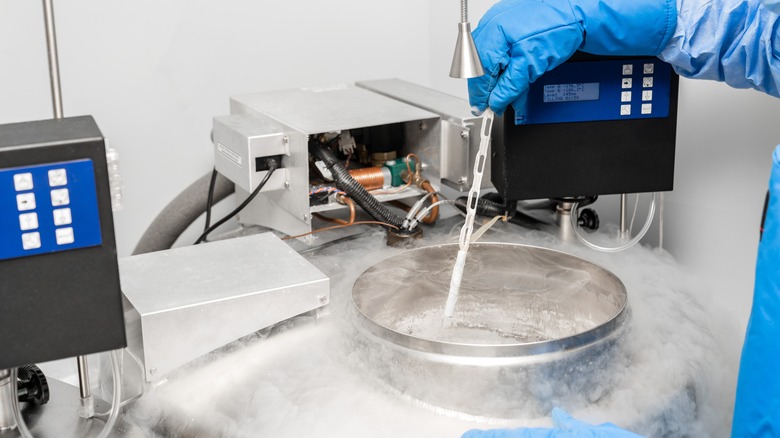
The root meaning of in vitro translates to something being in glass, which indicates how IVF is performed. In vitro fertilization is typically conducted by retrieving sperm from a man and eggs from a woman, then combining the two in glass tubes and other high-tech machinery in a scientific laboratory. After the respective reproductive materials have been created in a lab, a specified number of successfully created embryos are implanted into a woman's uterus. Unlike in vivo, the process of creating embryos outside of the body creates a distinction between the two types of fertility avenues.
In vitro fertilization is a research-backed fertility treatment, but it also comes with some potential drawbacks. Since several embryos are usually inserted when IVF is conducted, there is a likelihood of having a multiple birth, a term used to describe the pregnancy and birth of more than one baby at once, such as twins or triplets (via Mayo Clinic). The rates of premature birth, miscarriage, and ectopic pregnancy are also increased when it comes to conception through IVF.
Making decisions about fertility treatment
The Centers for Disease Control and Prevention reports that just over 2% of babies born in the United States have been conceived using assisted reproductive technology (ART), which includes in vitro fertilization, emerging in vivo technological methods, and other fertility treatments. There are nearly 500 clinics in the United States that offer ART procedures — and many medical professionals who specialize in working with individuals and couples wishing to pursue fertility treatment — who can help determine the best fertility treatment for you. For instance, IVF isn't an effective option for everyone, but it has been successful when underlying medical conditions like polycystic ovary syndrome (PCOS), male factor infertility (MFI), and blocked or improperly functioning fallopian tubes are determined to be the reason for infertility, per Forbes.
The decision to undertake the process of IVF or any other form of fertility treatment is one that should be consulted on with your healthcare provider, and it can be an experience that is both physically and emotionally demanding. Financial considerations must also be made given that an average round of IVF costs between $10,000 and $15,000 (via Penn Medicine). This number can increase since multiple rounds of IVF are often required to achieve successful implantation of embryos, which can compound the physical strain of daily injections required for the fertility treatment and the emotional weight of the process, says Forbes. When making your decision, be certain to factor in mental health support and self-care.