Ovarian Cysts Explained: Causes, Symptoms, And Treatments
People with female anatomy have two ovaries, located on each side of the uterus, attached to the fallopian tubes (via Mayo Clinic). The ovaries are responsible for the development and maturation of the eggs that get released during each menstrual cycle.
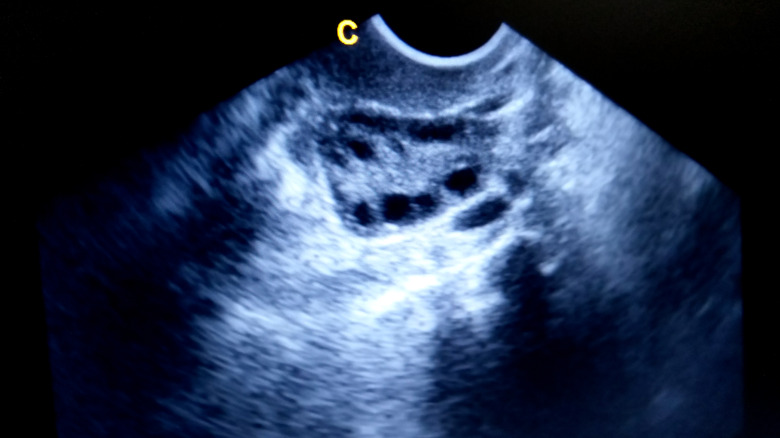
Sometimes, small sacs of fluid develop in or on the ovaries. These are known as ovarian cysts. According to the Office on Women's Health, a division of the Department of Health and Human Services, ovarian cysts are a common occurrence, and most cysts happen as a result of normal ovulation. However, about 8% of people with female anatomy will get large ovarian cysts at some point in their lives. In addition, some people will get ovarian cysts more frequently, usually because they have another medical condition.
Often, people won't even know if they have an ovarian cyst unless one gets found during a medical exam because they don't always cause symptoms. The majority of cysts don't pose any medical risk and will resolve on their own.
Here's everything you need to know about why ovarian cysts happen, the symptoms they can cause, how they should be treated, and the complications that can occur.
Functional cysts
The majority of ovarian cysts are functional cysts. According to the Office on Women's Health, there are two types of functional cysts and both form as part of the normal ovulation process.
When an ovary is preparing to release an egg during the monthly menstrual cycle, the egg is contained in a fluid-filled sac known as a follicle. Typically, this sac opens to release an egg. If it doesn't, then the sac continues to fill with fluid, causing a cyst known as a follicle cyst or follicular cyst.
When the egg is released as it should be, the follicle sac should decrease in size and develop the corpus luteum, an aggregation of cells that produces the hormones necessary to get another egg ready for the next menstrual cycle. According to New York-Presbyterian, sometimes, instead of decreasing in size, the follicle closes after it releases the egg. This allows the sac to continue to fill with fluid, causing a cyst known as a luteal cyst or a corpus luteum cyst.
Most functional cysts are harmless and will resolve within a few months without any treatment.
Ovarian teratomas aka dermoid cysts
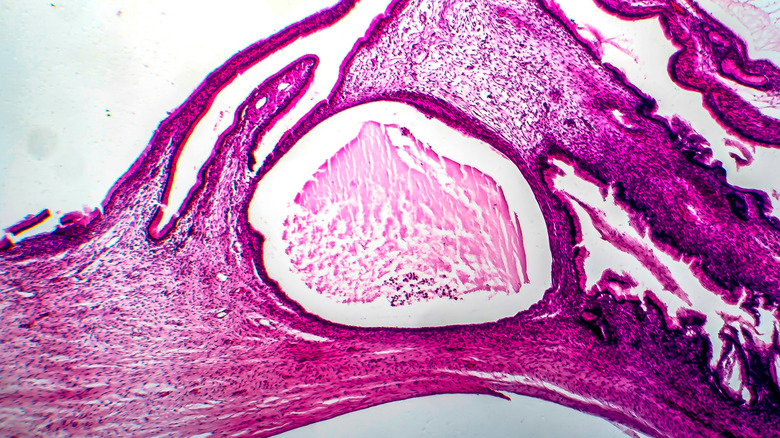
An ovarian teratoma is a specific kind of germ cell tumor, per the Cleveland Clinic. Though most people think of "cancer" when they hear the word "tumor," most ovarian teratomas are benign (non-cancerous). Teratomas are a rare kind of tumor that develops from the cells that make up the reproductive system. Because they're made from reproductive cells, which can form any kind of bodily tissue, teratomas can be filled with bone, teeth, hair, and/or muscle tissue. These tumors happen when there's a problem with the body's ability to identify which kinds of cells it's supposed to be making.
Teratomas can grow anywhere in the body, in people with female or male anatomy. In people with female anatomy, they're most commonly found on the ovaries. There are two types of ovarian teratomas – mature and immature. While mature teratomas are typically non-cancerous, immature teratomas can be cancerous. According to the National Library of Medicine, only mature teratomas are considered to be ovarian cysts, also called Dermoid cysts.
Though teratomas are the most common kind of ovarian germ cell tumor, they're still rare, accounting for just 20% of all ovarian germ cell tumors, which are also rare. Only about 1% of ovarian teratomas become cancerous.
Ovarian cystadenomas
Sometimes, the cells on the outside of the ovary reproduce abnormally and create cystadenomas. According to the National Library of Medicine, ovarian cystadenomas are technically tumors, like ovarian teratomas. However, when they're only filled with fluid and no solid tissue, they're considered ovarian cysts and are almost always benign.
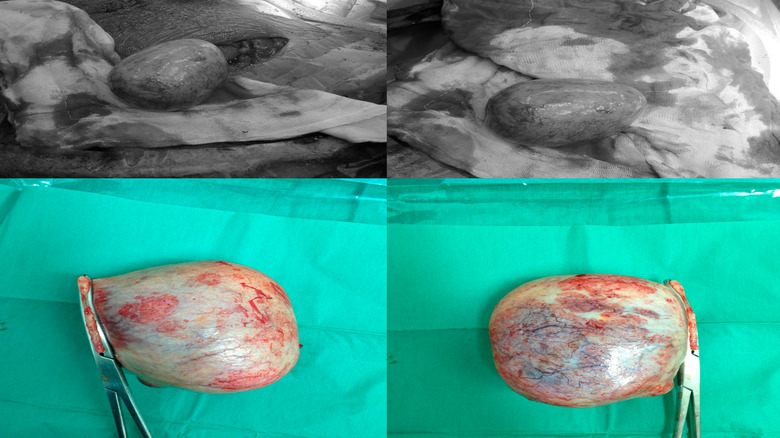
Ovarian cystadenomas can be filled with watery, clear fluid –- Serous Cystadenoma –- or a mucous-like fluid –- Mucinous Cystadenoma. Cystadenomas are typically between 1 and 3 centimeters in size, but they can grow quite large. Some cystadenomas are as big as 30 centimeters, though the average size is about 10 centimeters. Because these cysts can get so big, they often require surgical intervention to prevent complications. According to a case study published in the Cureus Journal of Medical Science, ovarian cystadenomas over 10 centimeters, often referred to as giant cysts, are extremely rare.
Ovarian cystadenomas are much more common than ovarian teratomas. Around 60% of all ovarian tumors are cystadenomas, and about 40% of all benign tumors are cystadenomas.
Ovarian endometriomas aka chocolate cysts
Endometriosis is an inflammatory reproductive disease in which endometrial tissue, similar to the tissue found inside the uterus, grows outside the uterus, per Medscape. Between 5% and 10% of people with female anatomy have endometriosis.
Studies have found that between 17% and 44% of people with endometriosis will get a specific kind of ovarian cyst called an endometrioma at some point in their lives. Ovarian endometriomas are cysts filled with old, thick blood, which makes them appear brown. That's why endometriomas are commonly called "chocolate cysts."
Experts don't yet agree on how endometriomas form on the ovaries. In people with endometriosis, the endometrial tissue that implants itself outside the uterus sheds and bleeds with each menstrual cycle. Some experts suggest that this accumulation of blood from endometrial tissue deposits on the ovaries, causing endometriomas. The shedding and bleeding of the endometrial tissue outside the uterus also damages the healthy tissue around the implants, causing lesions. Some experts theorize that these lesions cause endometriomas. Still, others propose that the presence of endometrial tissue on the cysts can transform functional cysts into endometriomas.
Regardless of how endometriomas form, they are considered a sign of severe endometriosis, according to the National Library of Medicine. Though endometriomas can be seen on transvaginal ultrasounds, the only way to confirm that an ovarian cyst is actually an endometrioma is by biopsying the tissue. Since most endometriomas require surgical removal, the tissue is biopsied after the cyst is removed.
Causes of ovarian cysts
Each kind of ovarian cyst is caused by a different biological process. According to UpToDate, ovulation is the most common cause of ovarian cysts because the majority of cysts are functional cysts. These cysts develop due to glitches in the ovulation process, such as when a follicle sac doesn't release an egg or the follicle sac closes before shrinking after the egg is released.
Ovarian teratomas or dermoid cysts, ovarian cystadenomas, and endometriomas are all pathological cysts. These cysts don't form as a result of the menstrual cycle like functional cysts, per London Women's Centre. Pathological cysts are caused by abnormal cell growth, like tumors. Though these cysts can be cancerous, they're often benign, just like functional cysts.
Multiple co-occurring medical conditions -– including endometriosis, Polycystic Ovarian Syndrome (PCOS), and pelvic infection –- can lead to the development of pathological cysts. Endometriosis causes endometriomas, while PCOS causes multiple pathological cysts to form at any time of the menstrual cycle, not just ovulation, when functional cysts form. Pelvic infections can also spread to the ovaries and cause pus-filled cysts. Sometimes, though, the origin of the abnormal cell growth that causes pathological cysts is unknown.
Symptoms of ovarian cysts
Most of the time, ovarian cysts are asymptomatic. According to Penn Medicine, many people don't even know they have an ovarian cyst until a provider discovers the cyst. This often happens when people are undergoing imaging tests for other medical issues, but can also happen during a routine pelvic exam.
People who do experience symptoms often report symptoms similar to those often experienced with the menstrual cycle. These include pelvic pain shortly before menses, achy pelvic pain throughout the menstrual cycle, abdominal bloating, and abdominal swelling. Some people also experience painful bowel movements, trouble urinating, soreness in the breasts, pain during sex, pain in the lower back or thighs, and pain during movement.
According to Cedars Sinai, the most common symptom of ovarian cysts is one-sided pelvic pain or a sensation of pressure on one side of the lower belly. Rarely people will experience spotting or bleeding between periods because of an ovarian cyst.
Cysts are more likely to cause symptoms when complications like rupture and torsion occur.
Diagnosing ovarian cysts
If you or your medical provider suspects that you have an ovarian cyst, the diagnostic process will often start with a physical exam, per Cedars Sinai. They'll likely perform a pelvic exam to determine whether you have swelling around one of your ovaries. Your provider may also feel that telltale swelling during a routine pelvic exam, which can be the first sign that you have a cyst if you weren't having any symptoms.
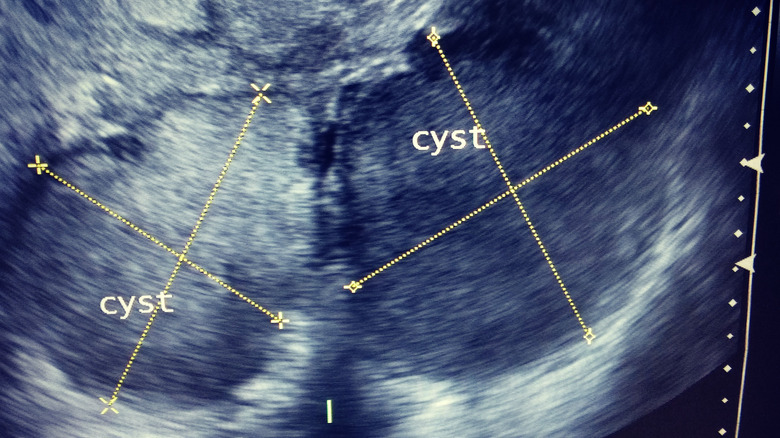
If the physical exam indicates that you might have a cyst, your doctor may order some tests to confirm the presence of the cyst and gather more information. According to a paper published by the Radiological Society of North America, the most common test is an ultrasound. Usually, an ultrasound allows your provider to visualize the cyst, determine its location, and estimate its size. Sometimes, your doctor will also be able to tell what kind of cyst you have based on how it looks on the ultrasound. If your doctor needs a better look at the cyst, they might order an MRI to get a more detailed picture.
Your provider may also order blood tests to check for hormone imbalances and markers that indicate the cyst could be bleeding or cancerous. Sometimes doctors decide to take a piece of tissue from your ovary and send it out for a biopsy. Usually, this is only done when your doctor is concerned the cyst is abnormal.
Treatments for ovarian cysts
According to the Mayo Clinic, the type of cyst and its size play a major role in determining treatment. Your age and the severity of the symptoms you're experiencing also influence the treatment plan.
The most common approach is actually holding off on treatment and observing the cyst over a period of a few months. Most cysts will resolve on their own without any intervention. If your cyst is small and isn't causing any symptoms, your doctor will likely recommend a follow-up ultrasound. You may have several ultrasounds scheduled at regular intervals so your doctor can see if the cyst changes in size or shape or if subsequent ultrasounds reveal any new information about what kind of cyst you have.
If your cyst is large, causing lots of symptoms, and/or it looks like a pathogenic cyst, your doctor may recommend surgery to remove the cyst. A cystectomy can usually be performed with a type of minimally invasive surgery called a laparoscopy. Small incisions are made on your abdomen, and your doctor inserts surgical tools through the incisions to remove the cyst. When a cyst is abnormally large, an open incision may be required. Usually, your surgeon will be able to remove the cyst without removing the ovary as well. However, in some cases, the ovary will also need to be removed.
If you get ovarian cysts regularly or get multiple cysts on the same ovary, your doctor may recommend hormonal medication to stop you from ovulating.
Size really matters
The majority of ovarian cysts are small, between one and three centimeters, according to the National Library of Medicine. Cysts this size are usually too small to cause symptoms and, more often than not, will go away on their own after a few months.
Some cysts can grow much larger, though. A paper on "giant cysts" published in the medical journal Cureus stated that cysts over 10 centimeters in size are "rare," though it's difficult to get an estimate of how often they occur because clear, standardized data about their occurrence isn't available. The largest ovarian cyst in medical history weighed 328 pounds. The authors stated that advances in diagnostic imaging, particularly ultrasounds and MRIs, have made it easier for doctors to diagnose and treat ovarian cysts before they become giant.
Ovarian cysts that measure between 5 and 10 centimeters are considered large, per UpToDate, and often require surgical removal. However, the size of the cyst is not indicative of whether or not the cyst is cancerous. Large cysts are often surgically removed because they are large enough to cause significant symptoms, and they increase the risk of complications like ovarian torsion.
Whether or not an ovarian cyst changes in size is also an important factor for diagnosis and treatment. If the ovarian cyst gets smaller over time, it's likely to resolve on its own. However, if an ovarian cyst grows over time and continues to grow, this may change the diagnosis or approach to treatment.
Ovarian torsion
When cysts get very large, the weight of the cyst can cause the ovary to move, twisting the fallopian tube, per Yale Medicine. This is called an ovarian torsion, and it causes sudden and severe pelvic pain, often accompanied by nausea and vomiting. Though ovarian torsion happens suddenly, sometimes people get intermittent cramps for days or weeks before the torsion happens. The cramps often occur because the ovary twists a little bit several times before the torsion occurs.
Diagnosing an ovarian torsion can be difficult because the primary symptom is severe pelvic pain, which can be caused by multiple conditions. When trying to figure out what's causing your pain, the medical providers will likely do an ultrasound, which can reveal the torsion.
Ovarian torsion doesn't happen often, but when it does, it's an emergency situation. The twisted fallopian tube often prevents blood from flowing to the ovary, and if the ovary is separated from its blood supply for too long, it can stop functioning or even die. So, the fallopian tube needs to be untwisted as soon as possible, and the cyst needs to be removed to ensure another torsion doesn't occur.
Usually, the torsion can be corrected during a minimally invasive laparoscopic surgery, and the cyst can be removed at the same time. However, if the torsion is complicated or the cyst is extraordinarily large, a full abdominal incision may be required. Sometimes, the ovary can't be saved and will also need to be removed.
Ruptured ovarian cyst
Sometimes, ovarian cysts will rupture. According to Johns Hopkins Medicine, a ruptured cyst doesn't always cause symptoms. Often the symptoms are mild and well managed with over-the-counter pain medications.
However, a ruptured cyst can sometimes cause severe pelvic pain on the side where the cyst burst, bleeding, and excessive fluid loss. If you experience a sharp, severe pain in your lower belly followed by vaginal bleeding not related to your menstrual cycle or excessive vaginal bleeding, you should seek emergency care. Though some bleeding can be normal with a ruptured ovarian cyst, excessive bleeding can lead to serious medical issues.
Ruptured cysts that cause excessive bleeding and fluid loss are often treated with intravenous fluids, pain medication, and sometimes a blood transfusion. In rare cases, a burst cyst can even require surgery. This only happens if medical professionals are concerned about excessive internal bleeding. Surgery for a ruptured cyst can often be performed laparoscopically. If they don't run into any complications, the surgery is relatively simple, and recovery is relatively quick and easy. You probably won't even need to stay at the hospital after the procedure.
Experts don't know why some cysts rupture while others don't. However, they are more likely to burst during strenuous exercise or sex. The majority of cysts don't burst.
Preventing ovarian cysts
Since the majority of ovarian cysts are functional cysts caused by normal ovulation, it's not possible to prevent ovarian cysts without preventing ovulation, per the American Academy of Family Physicians. As the Cleveland Clinic points out, most ovarian cysts will not cause any noticeable symptoms and will resolve on their own. So, there isn't really a need for prevention. However, your doctor may prescribe hormonal birth control if you get cysts frequently. Hormonal birth control can stop you from ovulating, which will help prevent the development of functional cysts. Scheduling regular pelvic exams so your medical provider can identify and monitor cysts is the best way to manage functional ovarian cysts.
Unfortunately, because pathological cysts form as a result of abnormal cell growth, per the London Women's Centre, they can't be prevented either. Some studies have shown that hormonal medications may help prevent endometriomas. Additionally, a paper published in Biomed Central Women's Health suggests that thorough surgery to remove all the diseased tissue created by pathological cysts may help prevent future pathological cysts.
Polycystic Ovary Syndrome (PCOS)
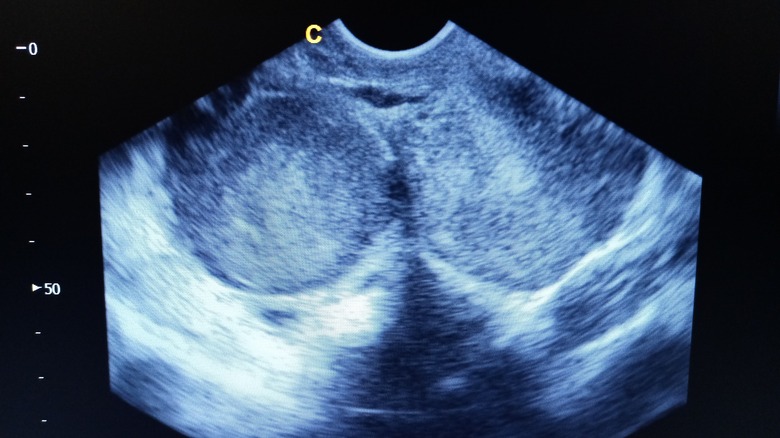
Some people who frequently get ovarian cysts have Polycystic Ovary Syndrome, commonly called PCOS. According to The American College of Obstetricians and Gynecologists, PCOS is a menstrual disorder that causes irregular menstrual cycles, infertility, and the frequent formation of ovarian cysts. Often, people with PCOS will get multiple cysts on each ovary.
Experts aren't entirely sure what causes Polycystic Ovary Syndrome. However, they do know that menstrual irregularities and high levels of hormones called androgens play a role in the development of the disease. Androgens are the hormones responsible for creating male characteristics like facial hair and a deep voice. When androgens are present in abnormally high levels in a person with female anatomy, they can disrupt the ovulation process. This can lead to the development of frequent, recurrent ovarian cysts.
Treatments for PCOS vary depending on what symptoms are present, pre-existing health conditions, and whether or not the person wants to get pregnant. Hormonal birth control pills that contain estrogen and progestin, often called combined birth control pills, are commonly used to treat PCOS. These pills regulate the menstrual cycle, which can help alleviate the symptoms of PCOS, including cyst formation.
The difference between ovarian cysts and ovarian cancer
According to the Ovarian Cancer Research Alliance (OCRA), the majority of ovarian cysts are not cancerous. Both functional and pathological ovarian cysts carry a small risk of being cancerous, but the vast majority of them are benign, or non-cancerous. Pathological ovarian cysts have a higher chance of being cancerous or becoming cancerous than functional ovarian cysts, but the majority of pathological cysts are still benign.
The major difference between ovarian cysts and cancerous growths is that cysts are fluid-filled, while cancerous growths are solid masses of tissue. Typically, ovarian cysts will also go away on their own without treatment, while cancerous growths will not.
The symptoms of an ovarian cyst and a cancerous ovarian growth can be similar. If you're experiencing persistent abdominal bloating and pain, pain during sex, and irregular periods, it's important to make an appointment with your doctor. They can use a transvaginal ultrasound to see if there are any growths on your ovaries and can often identify if those growths are just cysts or something else.
If your doctor finds a suspicious growth on your ovary or suspects ovarian cancer for any reason, they may order a CA125 blood test. This test detects a protein in the blood that is often elevated in people with ovarian cancer. However, this protein can also be abnormally high because of other gynecological conditions, so it's not a definitive test for ovarian cancer.