HPV Myths You Shouldn't Believe
According to the Centers for Disease Control and Prevention (CDC), human papillomavirus (HPV) is the most common sexually transmitted infection. Around 43 million HPV infections were diagnosed in 2018. This virus is transmitted through mucosa and skin cells and is of particular concern because, out of the 100 HPV genotypes known to date, 13 can cause cervical, anogenital, and head or neck cancers (via the World Health Organization). The high-risk strains HPV 16 and 18 cause roughly 70% of all cervical cancer. In 2002, the World Health Organization (WHO) estimated that HPV caused nearly half a million cervical cancer cases and a quarter of a million cervical cancer deaths globally.
Research suggests, however, that the HPV vaccine provides nearly 100% protection against pre-cancers caused by HPV (via the American Cancer Society). For this and other reasons, demystifying common misconceptions about HPV can save lives. Although it's estimated that around three out of every four people will be infected with HPV within their lifetime, misinformation and myths related to HPV remain common (via the American Sexual Health Association).
Myth: Only people who have many sexual partners can contract HPV
Contrary to popular misconceptions, any sexually active person can get HPV — transmission is not limited to those who have many sexual partners (via the American Sexual Health Association). Although having more sexual partners presents a higher level of risk that one of them will have contracted HPV (or another STI), anyone who has had sexual contact can contract the virus. Indeed, even among people with a history of only a few sexual partners, about 80% are estimated to have been infected with HPV. And even someone who has only ever had one monogamous sexual partner is still at risk if their partner may previously have contracted HPV. Overall, HPV is so ubiquitous that most every person who is sexually active at all will contract some type of HPV at some point in their lifespan (via the American Cancer Society).
Myth: You must have sexual intercourse to get HPV
Human papillomavirus (HPV) is the most commonly transmitted STI (via the CDC). That said, HPV is spread via close skin-to-skin contact, so it is possible to spread or contract HPV without having sexual intercourse (via University of Nevada). While condoms can reduce the risk of contracting HPV, they don't totally eliminate the risk because some genital skin remains uncovered by a condom (via the CDC). Research also indicates that HPV may be transmitted through finger, mouth, or even non-sexual skin or mucosa membrane contact (via Experimental and Therapeutic Medicine). Human papillomavirus can be found on contaminated gynecological equipment. Sometimes, HPV can be transmitted from mother to newborn via pregnancy or birth. This risk, however, is low.
The CDC suggests that an evidence-based approach to preventing HPV includes vaccination, using condoms (the correct way!) every time you engage in sex, and choosing monogamous sexual partners.
Myth: Men can't get HPV
Due to its link with cervical cancer, HPV may be most commonly associated with women or those who have a cervix. But HPV is not only found in women (via University of Nevada). While many people believe that men can only carry and spread HPV infection without any possibility of symptoms or effects, the reality is that men are also at risk of developing symptoms like genital warts or HPV-related cancer. HPV can lead to the development of penile, anal, or throat cancers in men.
According to the CDC, while most HPV infections clear on their own without causing any symptoms or health issues, men should be aware that prolonged infections can result in such illnesses. Genital warts may resemble small goosebumps or can be larger, raised, flat, or cauliflower shaped. They may increase or decrease in number, and can be treated but may return. It's important to note that warts themselves do not cause cancer. In fact, the types of HPV that can lead to cancer do not tend to cause genital warts. That said, though less common, it is possible for men to develop cancer due to certain HPV strains. Men who are immunocompromised are at an elevated risk of these cancers. Anal cancer is more likely in men who engage in anal sex, since they are at a higher risk of developing an HPV infection in that area.
Myth: People with HPV have symptoms
Many people believe that human papillomavirus (HPV) presents with obvious symptoms. This is a myth. Most people who are HPV positive are actually not even aware that they have the virus, and never develop any obvious health issues or symptoms (via the CDC). For many women, an HPV diagnosis is only arrived at after either an abnormal Pap result from a cervical cancer screening, or after the development of an HPV-related cancer.
According to Planned Parenthood, high-risk forms of HPV will largely present as asymptomatic, with no clear virus signs until serious health problems have developed. This highlights the incredible importance of regular medical care. Appropriate checkups and screenings can prevent cancer in cases where providers catch early warning signs. Be sure to talk to your primary care provider about appropriate screening for your gender and age if you are concerned about sexually transmitted infection prevention in general or HPV and related cancer prevention specifically.
Myth: If I got the HPV vaccine, I don't need a Pap
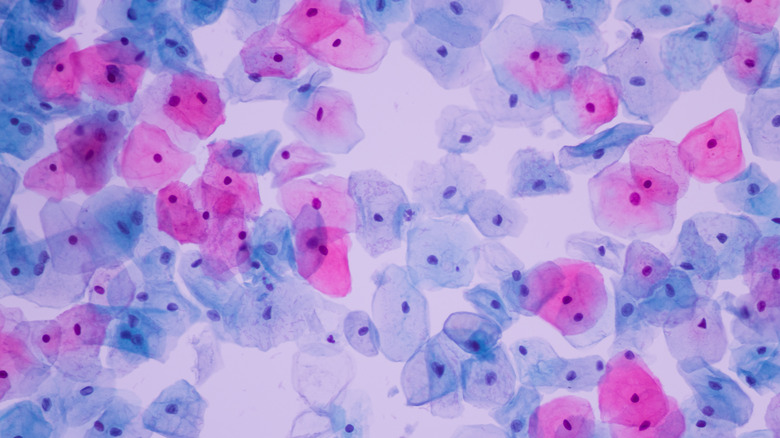
A Pap test, also known as a Pap smear, can detect precancerous cells or cervical cellular changes (via the CDC). The test is done in an outpatient office or clinic. The provider uses a plastic or metal speculum to open the vagina, examines the vagina and cervix, and collects a cervical cell sample. The sample is sent to a lab where it's screened for irregularities or HPV. The CDC currently recommends Pap smears beginning at age 21.
It is a false assumption that if you've received the HPV vaccine, you don't need Pap screening (via the National Cancer Institute). However, there is currently no vaccine that prevents all types of human papillomavirus (HPV). Since HPV is linked to potentially lethal forms of cervical cancer (per the CDC), Pap smear screening is recommended as an ongoing part of regular well care and cancer prevention.
Myth: Lesbians aren't at risk for HPV
Another dangerous cultural misconception is the idea that gay women cannot contract HPV, and that they therefore don't need to be screened for cervical cancer. This particular HPV myth is based on the false notion that human papillomavirus (HPV) can only be transmitted via penile-vaginal sex (via American Sexual Health Association). People often do not understand that the virus can be transmitted from one person to another through other forms of close skin-to-skin contact. Indeed, research from the University of Washington actually found HPV infection among lesbians, even some who had never had sexual contact with men. Although risk level may be lower for gay women than heterosexual women, anyone engaging in intimate contact skin-to-skin can contract HPV, and cervical cancer screening is still indicated for anyone with a cervix.
This is important information for the LGBTQ community in terms of reducing cancer risk. According to the American Cancer Society, a dangerous disparity of care exists for lesbian and bisexual women. Reasons for this include fear of potential discrimination, lower rates of insurance coverage among unmarried partners, and previous negative interactions with the healthcare system. These issues are highly concerning, since late screening can mean more advanced and less treatable cancers at the time of diagnosis.
Myth: If you get regular Pap smears, you don't need the HPV vaccination
Just as Pap screening is clinically indicated regardless of vaccination status, the HPV vaccine is still recommended even if you receive regular cervical care and screening such as Pap smears. The reason? Increased prevention equals decreased risk. An article published in Human Vaccines and Immunotherapeutics in 2018 indicated that although Pap smears have had a huge impact in terms of reducing the incidence of cervical cancer globally, vaccination is still critically important. Keep in mind that Pap smears do not screen for non-cervical HPV-related cancers. In the United States, there are roughly 12,000 new diagnoses of vaginal, vulvar, anal, and oropharyngeal cancer yearly in women and 19,000 annual cases of anal, penile, and oropharyngeal cancers in men. The HPV vaccine can not only help reduce someone's risk of developing many of these additional cancers, but can also prevent some aggressive forms of cervical cancer that would only be found in later stages via a Pap.
Myth: HPV is not common
Do you think HPV is not a risk for you personally? It may be worth rethinking that belief. You may not know it, but as many as 80% of people will contract HPV at some point in their lifetime (via the CDC). HPV is the most prevalent sexual transmitted infection. It's also the most common reproductive tract infection, according to the WHO. This is significant because cancer of the cervix is the fourth most frequent type of cancer globally, and approximately 95% of cervical cancer is caused by HPV. Issues of poverty are interwoven with the issue of cervical cancer, as around 90% of cervical cancer cases are diagnosed in low and middle-income countries. HPV is such a public health risk both nationally and internationally that in 2020 the World Health Assembly rolled out a global strategy toward eliminating cervical cancer. The strategy aims to prevent 300,000 cervical cancer deaths by 2030, and over 14 million deaths by 2070, through vaccinating 90% of girls by age 15, employing high-performance screening for 70% of women by age 35 and again by age 45, and by treating 90% of women with cervical disease.
Myth: If HPV doesn't cause symptoms, it's not a concern
Another rampant HPV myth is the notion that if you have no symptoms, there is no reason to be concerned about having HPV. Unfortunately, while high-risk HPV often does not present symptoms, it can still lead to cervical cancer (via Planned Parenthood). Regular well care and screening is critically important for this reason. The majority of people with high-risk HPV will not present with symptoms of infection at all until a serious health issue has developed, such as cervical cancer. Pap tests especially can save lives because they can detect abnormal cervical cells that may indicate a need for early intervention and treatment.
The same is true of high-risk HPV strains that cause other types of cancers such as those of the penis, vulva, anus, or throat: The HPV virus will likely be unnoticeable when first contracted. Be aware that although there is no cure for HPV, many times HPV infections do clear on their own in time. Besides regular preventive healthcare checkups, caring for your immune system and avoiding smoking can potentially decrease the risk of HPV developing into a long-term infection or cancer. Also, remember that the HPV vaccination can also prevent 90% or more of the cancers that HPV can cause (via the CDC).
Myth: An HPV diagnosis within a monogamous relationship indicates infidelity
It's important to note that HPV can surface in one partner during a monogamous relationship, and a new diagnosis does not mean that person has cheated (via the American Sexual Health Association). This is possible due to the fact that the virus can lay dormant within the body for years without symptoms. An HPV diagnosis only tells us that, at some point in the infected individual's life, they were exposed to HPV. There is no medical method for determining when an HPV infection was contracted or who it was contracted from.
The emotional aspects of an HPV diagnosis can be complex (via the American Sexual Health Association). Misinformation can cause people to feel awkward and vulnerable. Gathering accurate medical information and developing good understanding of HPV can help you feel more prepared to discuss an infection diagnosis with a sexual or romantic partner. You may want to talk to your healthcare provider about HPV causes, symptoms, and treatment. Remember that the majority of the sexually active population will be exposed to HPV at some point in time, and that contracting HPV is not a reflection of your character or identity.
Myth: The HPV vaccine causes tweens and teens to become sexually active
The CDC has reported that about 13 million people, including teens, contract HPV each year. However, HPV vaccination can prevent over 90% of HPV-related cancers. Since the 2006 introduction of the HPV vaccination in the U.S., high-risk, potentially cancer-triggering forms of HPV have decreased about 88% among teenage girls. Due to this, best pediatric practices have evolved so that more teens are getting vaccinated against HPV.
Despite evidence-based research data supporting the positive effects of administering the HPV vaccine to tweens and teens (via Human Vaccines & Immunotherapeutics), some people fear that the HPV vaccine encourages children and teens to engage in sexual activity before they would otherwise (per Harvard T.H. Chan School of Public Health). Researchers counter that HPV vaccination is recommended for ages 11–12 years of age not only to ensure it is in place before sexual activity, but also because vaccination before age 15 has been found to incite a much stronger immune response. It is also important to understand that HPV is not only sexually transmitted, but can be spread via skin-to-skin contact, sex toys, medical instruments, or even (though rarely) shared clothing. Studies repeatedly indicate no increase in sexual "promiscuity" in adolescents post-vaccination, and no correlation to increased sexual activity later on in life.