Dr. Nita Landry From The Doctors Talk Show On Sex, Periods, And Tips For Your Next Doctor's Visit - Exclusive Interview
Some doctors have a hard time talking about topics like sex with their patients, but not Dr. Nita Landry. According to Dr. Nita, "The reason that topics like sex and periods are considered taboo is because we were taught that they should be." We were told to not talk about these sorts of things, but the lack of conversation can end up being harmful to your health. Dr. Nita strives to approach these topics in a non-judgmental way to help make patients feel more comfortable in opening up.
Throughout her career, Dr. Nita has witnessed a lot of health issues be normalized that should have never been normalized in the first place. Given this disconnect between people and their health, Dr. Nita is on a mission to empower women with knowledge and an understanding of their bodies. She is a Board-Certified OB-GYN and medical expert and was a co-host on the Emmy Award-winning talk show "The Doctors" for six years.
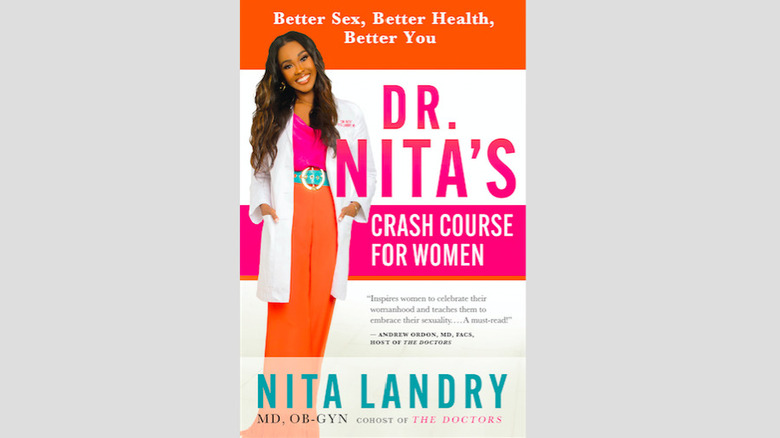
Her first book — "Dr. Nita's Crash Course for Women: Better Sex, Better Health, Better You" — just hit bookshelves nationwide. Dr. Nita sat down with Health Digest for an exclusive interview to talk about "taboo" topics like sex myths and periods, racial disparities in healthcare, when it's time to go to the doctor, and how to get the most out of your healthcare check-ups.
Dr. Nita noted that her use of the word "women" includes all people with uteruses.
Taboo topics should be encouraged
Can you share a little bit about your background and how you got into healthcare?
I am from Alexandria, Louisiana — a small town. When I was growing up, I was always interested in medicine and entertainment, but medicine was one of those things. I saw a lot of the women around me caring for other people, but they didn't take time to take care of themselves, and I saw their health suffer because of that. That was one of the things that made me interested in women's health, because although I was young and I couldn't articulate it, I was saying, "They're taking care of everybody else, but who's taking care of them?" The answer was nobody — nobody was, and that's why their health was suffering. I also saw a lot of teenage pregnancy, and I wanted to be in a position where I could be a source of encouragement, upliftment, and support for young ladies who found themselves in that position.
It's monumental that you brought women's health to mainstream media — important topics can be swept under the rug because they're considered taboo or uncomfortable, like sex and periods. Do you see this often in your own practice and work?
I see it when people initially walk in, but after the appointment with me, I definitely see a shift in that mentality. Here's why: The reason that topics like sex and periods are considered taboo is because we were taught that they should be. We didn't just grow up and say, "That's something we shouldn't talk about." People told us that.
When I approach these topics in a conversational way, using a tone that makes it clear that I don't think they're taboo topics at all, patients start to drop their guard. People want to have these conversations — which makes sense, because why would you want to suffer unnecessarily during periods or have bad sex when you could work with someone, with a trained professional like me, who can identify easy, practical ways to improve your sex life?
To answer your question, "Do I see it?" Yes, but aligning yourself with a clinician who makes you feel comfortable having those conversations that you traditionally thought of as quote-unquote taboo ... Approaching it in a different way can maybe not make you want to say, "I'm 100% sexually liberated now!" — I'm not saying that I take people from zero to a hundred necessarily — but definitely, the way you approach the subject matter matters. You have to find someone you feel comfortable talking to.
Three biggest sex myths dispelled
Let's dive into some of the "taboo" topics. In your professional opinion, what are the top three biggest myths that women believe about sex?
We've been taught that first comes desire, then comes arousal, and the grand finale is orgasm. We've been taught that if you don't experience all of those things, something is wrong with your sex life — and that's not true. Pleasurable sexual experiences can be very different from person to person, or even from experience to experience. Myth number one is that if you don't find yourself wanting sex spontaneously, there's something wrong with your level of sexual desire, and that's not true. There's something called spontaneous desire, and there's something called responsive desire. With spontaneous desire, that is a normal way to experience desire, but it's that you want sex out of the blue.
[With] responsive desire, which is also a perfectly normal way to experience desire, a person won't necessarily be wanting sex, but they will allow their partner to stimulate them, to arouse them first. Once they reach a certain arousal level, then they'll find themselves desiring sex. That's perfectly normal too, but people seem to think that responsive desire is almost like a second-place prize or it's not normal, whereas it is. That's myth number one — the whole concept that spontaneous desire is the only way to experience desire.
Myth number two is that all sex requires an orgasm. When you listen to sex experts, a lot of them tell people to focus less on orgasms and more on sexual pleasure overall. One of the best analogies I heard was when they equated it to eating out at a restaurant. They said, in a great restaurant experience, you walk in, you have bread, you have dinner, you have dessert; all of those things are important. They're all pleasurable and you're enjoying all of those things.
The orgasm is like dessert — the dessert is great, but you can still have a great dinner without dessert. Their point is [to] think of sex as the entire meal. If you're just saying "dessert, dessert, dessert," then you're missing out on all of those other pleasurable moments. You can absolutely have great sex without an orgasm. Not that I'm frowning upon orgasms — they're great too — but you can have great sex without having an orgasm. That's myth number two.
The third myth — and this specifically pertains to heterosexual relationships — is that vaginal penetration is the gold standard when it comes to sex. Most vagina-owners who are adults know all about the clitoris and they understand the importance of clitoral stimulation, but even when those women experience sexual pleasure with clitoral stimulation, if they don't experience sexual pleasure with just penetration, they're disappointed. It's important for women to lean into what works for them and know that some man told us that vaginal penetration was supposed to be the gold standard because that's what works for them.
That's great that that works for them, but this is a team sport. There are a couple of people here — or I don't know, do your thing, maybe more than a couple — but there's at least a couple of people here, and everybody deserves to be pleased. We can do some penetration for you, and then what are we going to do for my pleasure, if you're one of the 75% of women who don't experience an orgasm from penetration but can experience an orgasm from other things?
The truth about period pain
Let's talk about periods: Can you explain what causes period pain and the steps women can take to stop it?
Period pain can be broken down into two main categories: primary dysmenorrhea and secondary dysmenorrhea. With primary dysmenorrhea, your body produces hormone-like substances called prostaglandins, and those prostaglandins cause your uterine muscles to contract. When your uterine muscles contract, that can cause pain.
Secondary dysmenorrhea is when you have period pain because of an underlying issue. For example, endometriosis — which is when the inside lining of the uterus gets outside of the uterus — is the most common cause of secondary dysmenorrhea. The treatment is going to depend on the severity of your pain, your medical history, and your desires. To give you an idea of some of the common things that we use, a lot of times we'll use hormonal medications such as birth control, non-steroidal anti-inflammatory drugs, and heating pads, [which] are a lot of people's best friend when their period is happening.
I'm also a fan of something called a TENS device, and TENS stands for transcutaneous electrical nerve stimulation. These are inexpensive, non-invasive, medicine-free devices that work for a lot of patients with period pain. You can get them over the counter, and you can wear them under your clothes discreetly. A lot of patients have a lot of success with that, and I'm also a huge fan of pelvic physical therapy.
There are specially trained physical therapists who can help you to relax the muscles and retrain the muscles in the pelvis, and sometimes that can be very beneficial. There are a lot of different ways we can approach it, depending upon what's going on, but overall, if you are an adult and you are having period pain, I would recommend that you request a transvaginal ultrasound to make sure that there's not an underlying cause. If you have primary dysmenorrhea, which usually starts early on within a year of a person's period as opposed to later in life, then birth control, NSAIDs, and heating pads can be very beneficial. But if you have secondary dysmenorrhea, then it's probably not going to get better unless you treat the underlying cause.
One of the big things you can do to tell if you have primary dysmenorrhea versus secondary dysmenorrhea is remember that primary dysmenorrhea usually starts in adolescence, within one year of your first period. Secondary dysmenorrhea usually starts after the age of 25, although it's possible for it to start earlier. Teenagers can have endometriosis, for example, but thinking about when the pain started may give you a clue. That transvaginal ultrasound is going to be important. Although it won't identify every possible cause, it can help to eliminate some of the potential causes of secondary dysmenorrhea.
[For] people who want to do vitamins and things, we don't have a lot of information on it to prove that it works, but vitamin B1, vitamin B6, magnesium, ginger powder, things like that — sometimes people will find [those] helpful.
Racial disparities in healthcare
Are there any other red flags that you should be on the lookout for that your period is a problem and it's time to go visit your OB-GYN?
Period pain that doesn't resolve with treatment options like over-the-counter medications or a heating pad; if your pain lasts for more than a few days each month; if you're missing school, work, or parties because of your period; if you have a fever or if you have heavy bleeding along with your pain — all of those things should prompt you to talk to a healthcare professional.
October is Breast Cancer Awareness Month. A recent study by the American Cancer Society showed that while breast cancer death rates have dropped considerably, Black women continue to be 40% more likely to die from the disease. Do you consider racial disparities in medicine to be a public health emergency?
Absolutely. When it comes to disparities like this, a lot of people assume it's all about genetics or lifestyle choices, but that's 100% untrue. While those things play a role, study after study states that things like implicit bias, structural racism, inadequate access to healthcare — all of those things — come into play.
Can you talk about your experience with healthcare disparities?
After I finished residency, I became a traveling doctor, so I traveled across the country practicing medicine. As I picked different clinics and hospitals to work at across the country, I intentionally chose a lot of assignments with very different patient populations. Most of the assignments I chose were in clinics and hospitals that provided care for marginalized communities.
For example, I worked on Native American reservations that had a lot of patients who could not afford expensive medication. They would come in and I was like, "Why aren't you taking your medication?" The reason was they couldn't afford to buy food and buy medication — a lot of people have to pick. When I looked at the very different experiences of individuals who have access to any type of healthcare that they need and desire, and I compare that to people in marginalized communities, it's astounding.
You see situations where people are losing their life because their insurance company is saying, "No, they don't need this medication." These [insurance] people are not doctors. You say [to them], "Okay, well, what do you propose that we do?" They give us some suboptimal treatment option that's going to be beneficial for their bottom line.
We all know that it's not fair; it's not right. The value of a person's life has nothing to do with their bank account — we're all equal. But I've seen quite a number of health disparities, and it's definitely something that we need to work on in this country. We can do better; we should be doing better. The systems that we have in place to take care of individuals in marginalized communities are inadequate, and people deserve better. We can do better, and we're not.
Get the most out of your doctor's visit
Thank you for speaking to that. Do you have any tips for Black women to be prepared for their next trip to the doctor's office?
Black women should walk in being mindful of the fact that healthcare inequalities are present for Black women regardless of socioeconomic status. Black women are disproportionately impacted by a number of health issues. For example, compared to our white counterparts, we are generally at a higher risk for heart disease, stroke, cancer, asthma, diabetes, influenza, HIV and AIDS, and that's not even the complete list. Black women are three to four times more likely to die from pregnancy-related complications compared to white women, and you already mentioned the breast cancer statistic. It's important to note those things, but in spite of those facts, it is still possible for Black women to receive quality medical care.
Here are some things they can do. First of all, know your family history. Sometimes in families, people don't share their history because they don't want their family members to worry. That's problematic for two reasons: First of all, we want to be there to support our family members in times of need. But secondly, when you don't share your personal history with your family members, you're robbing them of an opportunity to be proactive in some cases. [If] your family member's experiencing a certain illness, that doesn't mean you'll definitely get it, but your family history can help your doctor determine if you're genetically predisposed to something. That may mean you need earlier screening or you need a certain type of genetic testing.
Also, know what's normal for your body and speak up when something changes. Actively seek doctors who make you feel heard and respected. One of the best ways to find a great doctor is word of mouth. If you're having a hard time finding someone who you click with, text your friends who live in the area and ask them if they have any suggestions. Once you find a doctor you like, also spread the word, because odds are, you know people who are looking for suggestions.
One other thing: Telemedicine is really nice now. In certain situations, depending upon what issue is being evaluated, if you can't find a local doctor who is giving you the care you need and deserve, maybe having someone in a location you can't visit personally look over your records might be helpful.
Also, ask questions. Sometimes doctors explain things in a way that makes it hard to understand. If you find yourself lost, don't just be lost — remember that we went to school for a long time to learn about this stuff. It's not like we hopped on Google a couple of days before you came and started reading up on your condition. We spent years and years and years and years. Sometimes people can feel a little embarrassed to ask questions, but don't be embarrassed — that's literally what we're there for. Remember, we literally spent years in school learning this, so we don't expect you to walk in knowing those things. There are no bad questions.
The last thing is: Trust your instincts. If you feel as though you're being subjected to healthcare that falls below what should be considered the standard of care, or you don't feel as though your concerns are being taken seriously, find a new doctor. I assure you that there are people out there who want to help you, who can help you, and you deserve that.
Dr. Nita's Crash Course for Women: Better Sex, Better Health, Better You
You just finished your first book, "Dr. Nita's Crash Course for Women: Better Sex, Better Health, Better You." Can you share your inspiration for writing the book and what you hope readers will gain from reading it?
A lot of health issues that should have never been normalized have been normalized. We talked about painful periods — one example is the only period you know is the period you have. You don't know what anybody else's period feels like. If your period has always been torture from period number one, then sometimes you can assume that's normal. Maybe you ask your mom or your grandma and they say, "All of the women in our family hurt like that." But it could be that all of you have a medical condition, such as endometriosis, where there's a genetic link that hasn't been properly diagnosed and you've all been suffering unnecessarily. One of the reasons I wrote it is because I did find that a lot of things have been normalized, and I wanted to give women answers that they need and let them know that those things weren't normal.
I also found that a lot of my family and friends who would call me with questions about their health aren't sure what questions to ask when they go to the doctor. I wanted to give women an easy-to-follow roadmap that says, "If you have this common issue, here's what you need to know before you go to your appointment. Here are some important questions to ask once you get there in order to get the answers you need and deserve."
Simply stated, I hope that readers will walk away feeling empowered to take charge of their health. I want women to have it all; we deserve it.
You can follow Dr. Nita Landry on Instagram and find her book, "Dr. Nita's Crash Course for Women: Better Sex, Better Health, Better You," on Amazon, at Barnes and Noble, and at your local independent bookstores.
This interview was edited for clarity.