Graves' Disease Explained: Causes Symptoms, And Treatment
You've probably heard of hyperthyroidism, which refers to an overactive thyroid that produces too much of the thyroxine hormone, leading to other issues like an irregular heartbeat and drastic weight loss (via the Mayo Clinic). Hyperthyroidism typically results from other underlying conditions, the most common of which is Graves' disease. While Graves' disease isn't very common (it only affects 2-3% percent of the population), it is usually the culprit behind hyperthyroidism in most cases, according to the National Organization of Rare Disorders (NORD). In fact, Graves' disease is responsible for 60-80% of hyperthyroidism cases (via the Cleveland Clinic).
Graves' disease affects more women than men and isn't a disease that discriminates based on country or region. Doctors suspect that the disease's prominence in women might have something to do with female hormones, according to MedlinePlus. Around 1.2% of the United States population suffer from hyperthyroidism, and while this small percentage might be causing you to feel like you're all alone in this illness, it's important to know that it can be diagnosed, treated, and even go into remission. Read on for everything you need to know about Graves' disease and how to treat it.
What is Graves' disease?
Graves' disease got its name from an Irish doctor named Robert Graves, who first diagnosed the condition in the 1800s. Graves' disease is, first and foremost, an autoimmune disease. An autoimmune disease develops when the immune system confuses healthy cells for invasive "bad" cells and starts attacking them (via the Cleveland Clinic).
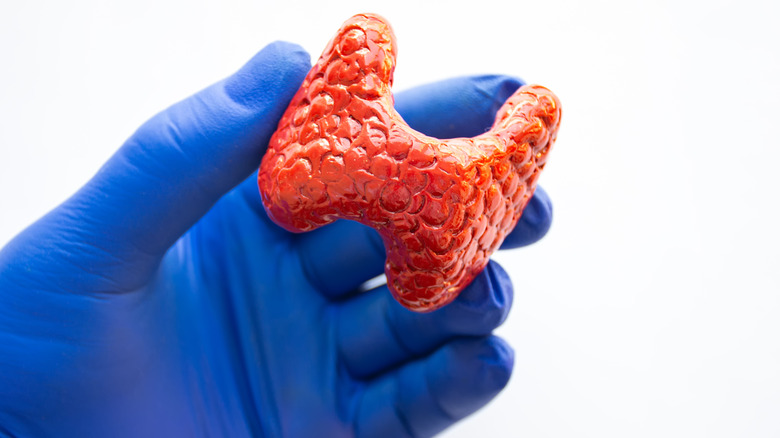
When you suffer from Graves' disease, the attack your immune system launches on your healthy cells is focused on the thyroid. The thyroid responds by producing more hormones than needed, which leads to hyperthyroidism, according to Medical News Today. The thyroid plays a vital part in our overall health. This small endocrine gland that resembles the shape of a butterfly can be found in the lower front part of your neck and works hard to control the speed at which your metabolism operates. When you suffer from hyperthyroidism, it has an adverse impact on the functionality of your metabolism (via the Cleveland Clinic).
Graves' disease tends to develop when people are between the ages of 30 and 50, but people of any age can develop this disease, although it's less common (via MedlinePlus). According to the National Institute of Diabetes and Digestive and Kidney Diseases, one in every 100 Americans suffer from this disease, most of which are women.
Causes of Graves' disease
The exact cause of Graves' disease is still a mystery to doctors. They know that, on the surface, the disease is caused by a glitch in the immune system. When it comes to figuring out what triggers this malfunction, however, doctors are still stumped, according to the Mayo Clinic.
While Graves' disease is often genetic, medical professionals also suspect that additional factors might be at play when it comes to the development of this condition. This includes environmental factors, as well as certain viral infections and bacteria. Doctors also suspect that hormonal fluctuations in females might be a potential trigger, but more research needs to be conducted to confirm these suspicions, according to MedlinePlus.
Graves' disease is, until proven otherwise, solely classified as an autoimmune disorder. Doctors found that patients with this disease have a protein called thyroid-stimulating immunoglobulin (TSI) in their system, which is produced by the immune system when it tries to attack the thyroid. TSI causes the thyroid to go into overdrive, producing more hormones than is normal. This typically leads to all the symptoms associated with Graves' disease.
Some people are more susceptible to Graves' disease
As with most diseases, some people are more prone to developing Graves' disease than others. Those who have family members who suffer from Graves' disease or other thyroid diseases like Hashimoto's disease are typically at a higher risk of developing this autoimmune disorder sometime in their lives, according to the National Institute of Diabetes and Digestive and Kidney Diseases. If you smoke, you're also making yourself more susceptible.
Those who suffer from existing autoimmune diseases also tend to be more prone to developing Graves' disease. People who suffer from type 1 diabetes are considered high-risk patients, as well as those who suffer from autoimmune gastritis (a condition where the stomach lining's cells are attacked by the immune system). Other autoimmune diseases that make you more susceptible to Graves' disease include rheumatoid arthritis and vitiligo. The Cleveland Clinic explains that people who suffer from celiac disease and lupus are also considered high-risk patients.
In some cases, those who have a family history of Graves' disease can develop the illness when they experience prolonged periods of physical or emotional stress, whether it be caused by illness or other traumatic life events. Those who are genetically more prone to the disease can also develop it while pregnant or after giving birth, according to the Mayo Clinic.
This is what Graves' disease does to your body
Since the hormones produced by the thyroid gland play a crucial part in many bodily functions, Graves' disease can cause a wide range of symptoms.
Typical symptoms associated with Graves' disease include feeling anxious and irritated, developing tremors in the fingers or hands, as well as fatigue and a change in sleeping patterns, according to the Mayo Clinic. Some people experience drastic weight loss while also seeing noticeable changes in their menstrual cycle. A lack of libido as well as erectile dysfunction can also be telltale signs of Graves' disease. Developing a sensitivity to heat and noticing a change in the size of your thyroid are also warning signs you shouldn't ignore, as are bulging eyes and the development of red, thick skin on your feet and shins. Having more bowel movements than normal and experiencing heart palpitations are also common symptoms of Graves' disease.
Per the Cleveland Clinic, if left untreated, Graves' disease can affect the strength and density of your bones as well. Having an excess of the thyroxine hormone in your system accelerates bone loss, according to the British Thyroid Foundation, and this eventually leads to osteoporosis. Treating the abnormal levels of thyroxine in the body can help remedy the rate at which bone loss occurs, and patients might be able to regain some of their bone strength. Aside from your bone health declining, Graves' disease can also affect your heart, liver, skeletal muscle, skin, and eyes.
How is Graves' disease diagnosed?
Diagnosing Graves' disease requires several tests and scans, but your doctor will typically start off by asking you if you have any other family members who have been diagnosed with the condition. Then, they will put you through a series of tests to confirm whether or not you have the disease, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
Your doctor will typically order a blood test first. This will indicate whether your thyroid hormone levels are higher than normal and if there is any thyroid-stimulating immunoglobulin (TSI) in your system. Next, your doctor will order a radioactive iodine uptake test that will specify whether your thyroid is absorbing more iodine than normal from the bloodstream. High absorption levels are typically an indication of Graves' disease.
Alongside the radioactive iodine uptake test, your doctor will likely order a thyroid scan as well. This will allow them to look at the iodine patterns in the gland, and if it shows up throughout your thyroid, you likely suffer from Graves' disease. Other iodine patterns can also indicate hyperthyroidism, but in these cases, the underlying cause is usually something else, like nodules. If you're pregnant and can't undergo a radioactive iodine uptake test, your doctor will order a doppler blood flow measurement. This test uses sound waves to measure whether there is an abnormal amount of blood flow to your thyroid, which is also indicative of Graves' disease.
Graves' disease can be treated in various ways
Thanks to modern medicine, there are various ways in which Graves' disease can be treated. Most of them are focused on stabilizing the thyroid's function to help ease symptoms.
Your doctor will likely prescribe antithyroid medications that can manipulate the amount of iodine your thyroid produces or block production entirely. These medications are typically prescribed long-term, but can also be prescribed ahead of surgery or radioiodine therapy, according to Mount Sinai.
Another, more drastic route your doctor might suggest is taking radioactive iodine. This medication works to damage the tissues of your thyroid while leaving the rest of your body unharmed (via GoodRx Health). Once the thyroid is damaged, it starts to produce less iodine, leading to hypothyroidism (and thus curing hyperthyroidism). It is important to note that you'll need to take thyroid hormone medication for the rest of your life after undergoing this treatment, and that you can't get pregnant or breastfeed while taking it.
Other medications may be prescribed to treat symptoms related to Graves' disease, like anxiety, a rapid heart rate, and sweating. Typically, your doctor will prescribe beta-blockers to keep these symptoms under control.
Some patients develop Graves' ophthalmopathy and dermopathy
Graves' disease on its own is already a pretty tough condition to deal with, but about 30% of people diagnosed with the disease go on to develop symptoms of Graves' ophthalmopathy, which affects the eyes, according to the Mayo Clinic.
Symptoms typically manifest as redness and inflammation in the eyes. Patients also tend to develop a sensitivity to light and experience dry or watery eyes, as well as eyelids that retract or become swollen. Patients may also experience irritation and notice that their eyes develop a bulging look, according to Medical News Today. Graves' ophthalmopathy increases the pressure on the optic nerves in the eye, and if left untreated, the patient can develop double vision and even lose their sight completely. Doctors are still trying to figure out why the eyes are affected by Graves' disease.
In addition to developing eye problems, Graves' disease can also cause skin issues (known as Graves' dermopathy). This condition typically shows up on the tops of the feet and the shins, causing the skin to become thick and red. Patients may experience itchiness in the affected areas, and in some cases, this condition can be quite painful. It's less common than Graves' ophthalmopathy, though. Only 4% of Graves' disease patients develop this condition, according to GoodRX Health. People who suffer from Graves' dermopathy sometimes develop acropachy as well, which is a condition where the fingertips or toes swell and nails become curved.
Graves' disease can lead to additional complications
One of the most concerning complications of Graves' disease is the development of heart problems. When Graves' disease isn't treated properly or a patient doesn't receive any treatment at all, they might develop arrhythmia, more commonly known as an irregular heartbeat. This can be dangerous and put you at a higher risk for life-threatening heart conditions like heart failure and stroke, according to the Cleveland Clinic. Graves' disease can also affect the menstrual cycle and cause fertility issues and complications during pregnancy, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
Patients who suffer from Graves' disease are also at risk of developing thyroid storm. This is a very serious condition that occurs when thyroid hormone levels skyrocket. Symptoms typically include a fever, impaired concentration, increased heartbeat, vomiting, sweating, and diarrhea. In some cases, patients have seizures and fall into a coma (via Drugs.com). Failing to take thyroid medication as prescribed or stopping it altogether can cause thyroid storm, as well as untreated infections. Some medications may also trigger this condition.
Graves' disease can affect pregnancy
Those with Graves' disease who would like to become pregnant need to keep in mind that they'll have to be extra vigilant and see their doctor regularly.
Graves' disease can complicate pregnancies, since the fetus' healthy development heavily depends on a fully functioning thyroid. The thyroid fulfills a crucial part in developing a fetus' nervous system and brain, and if Graves' disease is not kept in check during pregnancy, it can harm both the mother and her unborn baby, according to the Cleveland Clinic.
Some complications that can arise due to high thyroid hormone levels include miscarriage, premature labor, and low birth weight. The baby might also develop hyperthyroidism. The mother also faces some risks, like developing high blood pressure (referred to as preeclampsia) and suffering congestive heart failure. To ensure the safety of both the mother and her baby, doctors require regular checkups so they can keep an eye on the mother's thyroid hormone levels.
Your diet can affect Graves' disease
Since Graves' disease leads to an overactive thyroid, it's important that you limit your intake of foods that contain iodine — your body already has an excess of it, and adding more through your diet is looking for trouble, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Avoid foods like dulse, kelp, and seaweed, and make sure you don't take any supplements that contain iodine. Your doctor can advise you on what foods you need to limit or avoid altogether.
As for the type of foods that can help you manage Graves' disease, Healthline recommends you eat plenty of calcium-rich foods (think almonds, broccoli, okra, and kale) since Graves' disease can cause your body to absorb less calcium than normal, leading to weak bones. Adding sufficient amounts of vitamin D to your diet can help your body better absorb calcium. Aside from getting enough sunlight, load up on foods like mushrooms, cod liver oil, tuna, and salmon.
While magnesium-rich foods can help the body absorb calcium, it also plays a vital role in keeping symptoms of Graves' disease at bay, and a deficiency can intensify symptoms, according to a 2018 study published in Scientific Reports. Add avocados, legumes, pumpkin seeds, and dark chocolate to your diet. Last, but not least, make sure you consume enough selenium since a lack of this mineral can increase your risk of developing Graves' ophthalmopathy. Brown rice, sunflower seeds, and brazil nuts all contain selenium.
There are things you can do to manage Graves' disease
While dealing with Graves' disease can be pretty daunting, there are some things you can do to manage the condition and ease symptoms as much as possible.
The best thing you can do to manage Graves' disease is to ensure you take your medication as prescribed by your doctor and don't miss any follow-up appointments. Your health depends on it. Drugs.com recommends you quit smoking if you're a smoker and try to refrain from being around secondhand smoke, since this can trigger Graves' ophthalmopathy or intensify the condition if you already have it.
If you do suffer from Graves' ophthalmopathy, wearing sunglasses outside can help you deal with any light sensitivity. Another great tip is to slightly elevate your pillow at night to help lessen the swelling of the eyes. Sometimes, doctors recommend that patients with Graves' ophthalmopathy use tape to keep their eyes shut while they sleep. This can work wonders to keep your eyes from drying out throughout the night.
Graves' disease can potentially be treated with surgery
If all other treatments fail, your doctor might recommend you undergo surgery to help treat Graves' disease. Surgery is usually treated as a last resort: If a patient has a large goiter, struggles with severe symptoms, or for some reason can't undergo radioactive iodine treatment or continue taking antithyroid medications long-term, doctors tend to recommend surgery (via GoodRx Health).
When performing the surgery, the surgeon might remove your entire thyroid or only a part of it. It all depends on how severe your symptoms are, according to Medical News Today. If the doctor removes the entire thyroid, the chances of hyperthyroidism recurring are practically zero. If only a part of your thyroid is removed, your chances of developing the condition again are only about 8% five years post-surgery. If only part of your thyroid is removed, the remnants can still perform the functions needed, but if the entire thyroid is removed, you'll have to take thyroid hormone medication to help your body function normally.
Surgery is the best way to get rid of hyperthyroidism quickly and permanently, but keep in mind that you might be left with some scarring. You'll also likely have a hoarse voice and neck pain post-surgery, which is caused by the breathing tube the doctor inserts during the procedure.
Graves' disease can go into remission
Graves' disease can seem like an uphill battle at times, but the good news is that it can go into remission with the right treatment. In fact, you might be back to your old self within one to two years if you take antithyroid medication as prescribed, according to GoodRx Health.
Doctors monitor a patient's antibody and thyroid hormone levels during this time to ensure that they return to normal before ending treatment. Typically, between 40% and 50% of patients who undergo this treatment end up in long-term remission, or are at least symptom-free for up to a year.
Sometimes, Graves' disease returns after treatment, and while this can be disheartening, there are other options if antithyroid medications aren't doing the job. If the disease continues to recur, your doctor will likely suggest you stay on medication long-term or undergo radioactive iodine treatment or surgery.
You could volunteer to take part in clinical trials for Graves' disease
New research is continuously conducted to better understand Graves' disease and how to treat it, and Graves' disease patients have the opportunity to volunteer for clinical trials that aim to find better and more effective treatments, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
Research mainly focuses on creating new medications to treat Graves' disease and its related conditions like Graves' ophthalmopathy. Doctors also use what they learn during clinical trials to better understand Graves' disease and figure out ways they can prevent it from occurring altogether. Clinical trials are the only way new medications and treatments can be discovered, and in order for them to be successful, they need volunteers who represent those who suffer from Graves' disease, as Griffin P. Rodgers, director of the NIDDK, explains in a video.
If you're interested in helping doctors find improved ways to treat Graves' disease, you can speak to your doctor about joining a clinical trial. They can help you choose one that's right for you.