Everything You Should Know About Hormone Therapy For Transwomen
When a person's gender identity doesn't match their sex assigned at birth, which is usually determined by the genitalia they're born with, they are transgender. According to Gender Spectrum, gender encompasses a person's internal understanding of their gender, their experience of their body, and the way they present themselves socially based on gender roles. Gender is not determined by the features of a person's body. People who were assigned male at birth, typically because they were born with a penis — whose gender is actually female — are trans women (Gender Spectrum). Many trans women choose to identify simply as women.
Trans women figure out that they're not cisgender — the term used to describe people whose gender matches their sex assigned at birth — in many different ways, as an article in Them details. Not all trans women know that they're trans from a young age. Some of them don't figure out that their sex assigned at birth doesn't match their gender until they're adults. However, some children express a strong desire to behave like the opposite sex from a young age. Everyone's path is different.
Likewise, some trans women choose to wear feminine clothes and makeup while others don't. Some trans women choose to change their bodies to align with their gender while others don't. Those who do want to change their bodies often undergo hormone therapy and sometimes surgeries. Here's everything you should know about hormone therapy for trans women.
Social transition vs. medical transition
When a child, teen, or adult understands that they're trans, they may decide to start transitioning. Trans Families outlines four different kinds of transitions that trans folks might choose to undertake in order to live their most authentic lives: social transition, legal transition, medical transition, and surgical transition.
Social transition is typically the first step people take to express their gender to themselves and others. It refers to the ways people change their gender presentation — the way they look and/or dress — and their gendered actions, like which bathroom or locker room they use. Trans girls or women may start their social transition by wearing feminine clothes, experimenting with makeup, letting their hair grow long, or wearing feminine wigs. They may also start participating in activities that are typically perceived as feminine and using spaces that are usually reserved for women. Some trans women will also choose to change their names and/or pronouns and ask family members, friends, and others to use their chosen name and pronouns.
Legal transition involves going through the legal processes required to change name and gender on identifying documents.
Medical transition refers to the use of medical interventions, like hormone therapy, to change the body. Many trans girls and women will choose to use hormones to change their body shape, develop breasts, and decrease their body hair. Some trans women's medical transitions also include surgical procedures, but some choose to just take hormones.
Choosing to medically transition
Not every trans woman chooses to medically transition, as Buzzfeed found when they asked several trans folks about medically transitioning. Some said that social transition was all they wanted. Many said that they didn't feel like there was anything "wrong" with their bodies or the body parts they were born with. A few of the Buzzfeed respondents pointed out that a common misconception about being trans is that every trans person feels like they're in the wrong body.
However, many trans people do experience distress over the fact that their anatomy doesn't match their gender. Sometimes the distress is so extreme that it merits a diagnosis of gender dysphoria. According to a paper published in the medical journal Psychosomatic Medicine, gender dysphoria is "body dissatisfaction — resulting from the discrepancy between 'assigned' sex at birth and experienced gender." Many trans people with gender dysphoria choose to medically transition in order to change their bodies to align with their gender. Medical transition, often preceded by and along with psychotherapy, is considered the standard treatment for gender dysphoria.
That paper explored how medically transitioning with hormone therapy and/or surgical interventions impacted body dissatisfaction in trans people with gender dysphoria. Unsurprisingly, the study found that trans people with gender dysphoria who chose to medically transition reported much lower levels of body dissatisfaction once their bodies began to change as a result of medical transition.
So, many trans women chose hormone therapy as a way to express their true gender.
Hormones trans women may choose to take
Hormone therapy looks different for each trans girl or trans woman. A paper published in the medical journal Australian Prescriber states that the hormones used vary depending on age and medical history.
For trans women, hormone therapy usually includes a combination of estrogen and anti-androgens, which block the natural production of masculinizing hormones. Some doctors prescribe progesterone in addition to estrogen and anti-androgens. According to Trans Care British Columbia, progesterone may aid in breast development and boost libido. However, research has not proven these benefits yet. Estrogen and anti-androgens can be taken as pills. Alternatively, estrogen can be administered via an injection, patch, or cream.
For trans girls, the approach to hormone therapy is quite different. Instead of starting on estrogen and anti-androgens (as the first stage), trans girls start on gonadotropin-releasing hormone (GnRH), which essentially blocks the effects of natural puberty. If gonadotropin-releasing hormone doesn't work well enough on its own, anti-androgens can be added to the hormone therapy regimen.
The second stage of hormone therapy for trans girls involves going on estrogen and anti-androgens, if they weren't already on an anti-androgen. The timing of the second stage of hormone therapy is less about whether puberty is complete or the age of the trans girl, and more about their readiness and capability to consent to hormone therapy. Trans girls should work closely with a medical professional, a therapist, and their families to determine when they're ready to move into the second stage of hormone therapy.
Physical changes during hormone therapy
The primary goal of hormone therapy for trans girls and women is to change their bodies so they present as their gender rather than their sex assigned at birth. According to the Cleveland Clinic, the physical changes initiated by a hormone therapy regimen depend on which hormones are taken.
Anti-androgens, which block the natural production of male hormones, will gradually change the secondary sex characteristics, muscle mass, and hair on the body. As the testosterone levels lower, the testicles get smaller, muscle mass decreases, and facial hair gets thinner. Most people will also experience a drop in libido and a decrease in erections.
Estrogen will gradually change the distribution of body fat, giving the body a more feminine shape. More fat will settle in the hips, face, and buttocks. Estrogen also causes the skin to soften and breast tissue to increase, leading to the development of breasts.
The timing of these physical changes vary from person to person. GenderGP states that the first physical changes will likely be a decrease in erections and decreased libido, which can start as early as one month on hormones. Skin changes, body fat redistribution, decreased muscle mass, shrinking of the testicles, and breast growth can start anywhere between three and six months after starting hormone therapy.
Emotional changes during hormone therapy
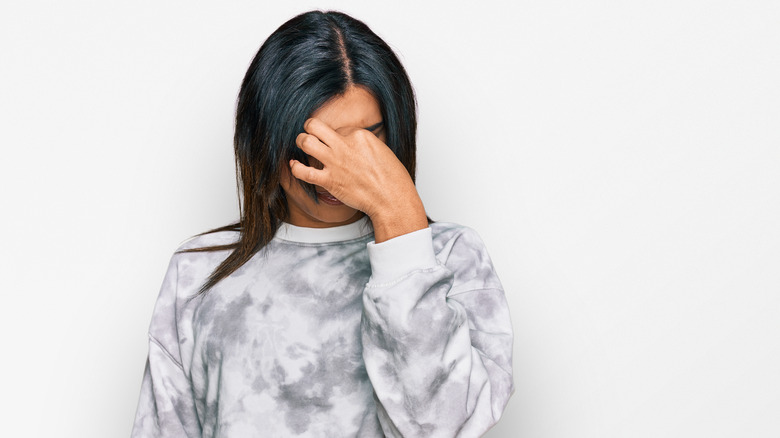
Every trans woman will have a different experience with emotional changes as a side effect of hormone therapy, per University of California San Francisco's Transgender Care Program (UCSF Trans Care). Anyone who remembers what puberty was like knows that it being an emotional rollercoaster is an understatement. Unfortunately, the "second puberty" caused by hormone therapy can be similar for some people.
Some trans women will experience a wider range of emotions than they did before starting hormone therapy, and they may feel those emotions more intensely. Some may also have mood swings and increased depression and anxiety. Those with existing mental health issues should have regular contact with a therapist while undergoing hormone therapy. Most people who do experience big mental health shifts find that their mental health stabilizes over time, as their body gets used to the new hormones.
Overall, gender-affirming hormone therapy has been shown to have a positive impact on mental health. A meta-analysis of 20 studies on the relationship between gender-affirming hormone therapy and mental health found that people who underwent hormone therapy reported that their quality of life improved and that their depression and anxiety symptoms decreased.
Hormone therapy and voice changes
Though feminizing hormone therapy causes a wide range of physical changes, it doesn't have any effect on the pitch of the person's voice, per a feature on vocal feminization by WBUR Boston. For many trans women, their voices give away the mismatch between their bodies and their gender. Since trans women can't rely on hormone therapy to change their voices the way trans men can, they have to seek other solutions.
Dr. Kim Hyung-tae, the director of the Yeson Voice Center in Korea, outlined the current approaches to vocal feminization in a paper for Dove Press. One option is surgical alteration of the vocal cords. This procedure may include shortening the vocal cords, making them thinner, and reducing the tension on the vocal cords. The end result is a higher-pitched voice.
However, pitch is not the only thing that distinguishes voices heard as male from voices heard as female. Adrienne Hancock, assistant professor of speech at George Washington University, told WBUR that men and women have different speech patterns, use different tones based on the situation, and choose different words to convey the same concepts. So, trans women need more than just a higher voice. They need to learn to speak like women.
To learn this crucial skill, many trans women turn to voice coaches and speech language pathologists. Hyung-tae asserts that a combination of surgery and consistent voice coaching produces the best results.
Hormone therapy and fertility
About half of trans women want to have biological children, according to a paper published in the medical journal Translational Andrology and Urology. Consequently, the impact of feminizing hormone therapy on fertility is an important factor in deciding whether or not to pursue medical transition and when to start hormone therapy.
Further research needs to be done to determine how puberty blockers impact sperm production. However, if puberty blockers are stopped, research has shown that sperm production usually returns to normal.
When trans women take estrogen and anti-androgens, their testosterone levels dramatically decrease, which changes the production of sperm. Research has shown that some trans women completely stop making sperm and experience testicular atrophy as a result of long term hormone therapy. However, some trans women only see a decrease in sperm production.
Though hormone therapy, especially long term hormone therapy, can potentially lead to infertility, this doesn't mean trans women can't have biological children. Studies have shown that trans women who stopped hormone therapy for several months were able to produce viable sperm samples that could be used in assisted reproductive procedures. So, even trans women who have started hormone therapy may be able to have biological children.
Trans women can also opt to freeze their sperm for later use before they start hormone therapy. This is the best route for trans women who think they may want biological children since their sperm production hasn't been impacted by hormone therapy.
Accessing hormone therapy as an adult
People over the age of 18 who want to start gender-affirming hormone therapy can start the process by speaking with their primary care doctor or getting a consultation with an endocrinologist or a gynecologist who specializes in trans healthcare, per the Cleveland Clinic.
In many states, people who want to start hormone therapy can head to their local Planned Parenthood clinic. A Planned Parenthood medical provider works with them to develop an appropriate treatment plan and prescribe the hormones that will best meet their transition goals. However, trans care isn't available at Planned Parenthood in every state.
For those who have trouble accessing trans healthcare in person, online services like Folx, Plume, and True U Clinic provide virtual transition care. For each of these programs, trans women can pay either a monthly subscription fee or a per service fee. The service hooks them up with a medical professional that specializes in gender-affirming care. Via a virtual appointment, the medical professional will assess transition goals and order blood tests. At a follow up appointment, they'll review those results and prescribe hormones as indicated. The hormones are shipped directly to the patient's home, often in nondescript packaging to ensure privacy.
Many medical professionals and insurance companies require trans women to attend therapy before starting hormones. These sessions allow trans women to explore their desire to medically transition, receive a diagnosis of gender dysphoria, and ensure that they can provide informed consent to begin hormone therapy.
Accessing hormone therapy as a child or teen
Getting gender-affirming hormone therapy is much harder for adolescents and teens. A feature on trans children and teens in The Conversation that explored access to gender-affirming care stated that there are myriad reasons why children and teens have trouble accessing hormone therapy. These could be anything from unsupportive family members to lack of basic healthcare to anti-trans legislation.
Andrea James, filmmaker and activist who runs Transgender Map, one of the longest running websites on gender-affirming care, stresses that the safest way for trans children and teens to access hormones is with the help of their parents (or guardian). If trans girls have parental support, they can have a parent accompany them to an appointment with their primary care doctor, an endocrinologist, or a gynecologist who specializes in trans care.
However, James acknowledges that not everyone can safely come out to their parents or ask for help seeking gender-affirming care. She suggested that those who don't have parental support start by talking to their primary care doctor without their parents present or going to Planned Parenthood.
However, many medical providers will not provide gender-affirming care without parental consent. And online services like Folx, Plume, and True U Clinic require proof that people seeking their services are over 18. Trans children and teens with unsupportive parents may have to wait to receive hormones until they turn 18 if they cannot find a medical provider in their state willing to prescribe without parental consent.
Insurance and hormone therapy
For many trans people, insurance coverage plays a major factor in whether they seek gender-affirming hormone therapy and how they access hormones. One study published in Annals of Family Medicine found that trans folks face significant barriers to getting hormone therapy covered by insurance.
Trans people are often discriminated against in the workplace and hiring process, leading to high levels of unemployment, leaving them uninsured. Others have trouble affording adequate healthcare and remain uninsured or underinsured regardless of employment status. Those who were uninsured were less likely to start hormone therapy, even if they wanted to.
About 9% of the trans folks involved in the study were taking hormones that had not been prescribed by a medical professional. Some of those people were uninsured, but some of them were taking non-prescribed hormones even though they had insurance coverage. The researchers found that around 20% of insured people who tried to get their insurance to cover their hormone therapy had their claims denied and sought out non-prescription hormones.
Insurance coverage is highly dependent on the insurance company and the state laws around trans healthcare. However, as the National Center for Transgender Equality points out, healthcare discrimination based on gender identity is illegal on the federal level, and insurance companies denying medically necessary transgender healthcare is discriminatory.
Many insurance companies have complicated pre-approval processes for covering hormone therapy, so trans folks need to get familiar with their health insurance plan and state laws before seeking hormone therapy.
Risks of hormone therapy for trans women
Though gender-affirming hormone therapy is generally considered safe, there are a few risks that trans women need to be aware of before starting hormones. According to the University of California San Francisco's Transgender Care Program (UCSF Trans Care), there isn't a lot of research about health risks of feminizing hormone therapy, especially the long term risks. Because of this, it's hard to determine the prevalence of certain risks
Risks that have been more frequently reported include blood clots, strokes, diabetes, and heart attacks. However, these risks are much higher for those with pre-existing conditions, people who start hormone therapy after the age of 50, and those who smoke. Smoking while on estrogen has significant health risks, so trans women should quit smoking before they start estrogen. UCSF's Trans Care program states that most of these risks can be mitigated by implementing lifestyle changes during hormone therapy.
Some research has shown that trans women have an increased risk of cancer, specifically breast cancer. However, per UCSF's Trans Care program, the research into this link is preliminary and more studies need to be conducted to prove this link.
According to the Mayo Clinic, additional risks of feminizing hormone therapy can include high cholesterol, high blood pressure, high potassium, nipple discharge, and hyperprolactinemia, a condition in which there's too much prolactin in the blood.
How long do trans women take hormones?
How long trans women stay on hormones depends on their goals for transitioning. According to Vancouver Coastal Health's Transgender Health Program some trans women will choose to stay on hormone therapy for the rest of their lives. Others will decide to stop hormone therapy altogether, change the dosages of the hormones they're taking or change which hormones they're taking.
Trans women who decide to have their testicles removed will produce very small amounts of testosterone after surgery. So, they can reduce or completely stop the amount of anti-androgens they're taking and reduce the amount of estrogen they're taking. However, trans women who get their testicles removed will need to take estrogen indefinitely to prevent osteoporosis.
According to a paper published in the journal Translational Andrology and Urology, some trans women stop taking hormones for a short period of time so their sperm can be harvested and preserved for assisted reproductive procedures like intrauterine implantation or in vitro fertilization in a partner with female anatomy. Typically, they can resume hormone therapy without issues.
Stopping hormone therapy
The majority of the changes that occur as a result of feminizing hormone therapy are reversible, per Vancouver Coastal Health's Transgender Health Program. So, if trans women decide to stop taking anti-androgens, estrogen, or both, most of the physical changes that happened while they were on hormones will slowly revert.
Muscle mass will begin to increase again, body fat will redistribute to a more male pattern, facial and body hair will start to regrow, sperm production will increase, and the testicles will begin to get bigger again. Trans women who stop hormones will likely experience an increase in sex drive and have more frequent erections.
The only permanent changes are breast growth and infertility. However, if trans women stop taking hormones shortly after starting hormone therapy, they may not have much breast growth and may not experience infertility. Not all trans women on hormones develop infertility, but harvesting and preserving sperm before starting hormones is the best way to ensure the ability to have a biological child in the future.
Gender confirmation surgeries
In addition to hormone therapy, some trans women choose to have surgical procedures to further align their bodies with their gender. According to the American Society of Plastic Surgeons, three common procedures trans women choose are facial feminization surgery, top surgery, and bottom surgery. Facial feminization surgeries involve shaping the face so the features are less masculine and more feminine. During top surgery, trans women undergo breast augmentation or shaping to make the breasts more feminine. Bottom surgery reconstructs the genitalia.
Mount Sinai Hospital states that each of these surgeries can involve a variety of procedures. Facial feminization surgery can include several different techniques including reshaping the bone structure of the face, rhinoplasty, altering the hairline, and reshaping the trachea. Top surgery may involve inserting breast implants, grafting fat from other parts of the body onto the chest, and shaping the breasts. Bottom surgery can include Orchiectomy, the removal of the testicles, and/or Vaginoplasty, the creation of a vagina, clitoris, and labia using the tissue of the existing genitals.
Additionally, some trans women choose to have vocal feminization surgery. This involves shortening the vocal cords to achieve a higher voice.