Humira Explained: Usage, Dosage, And Side Effects
Humira (adalimumab) is an injectable medication used in the treatment of several inflammatory and autoimmune conditions (per GoodRx). It is classified as a biologic disease-modifying anti-rheumatic drug (DMARD) and works by blocking the activity of a specific inflammatory protein called tumor necrosis factor (TNF) alpha.
Humira has been in use for over 20 years (via Drugs.com). Since its FDA approval in 2002, Humira has continued to receive additional use cases, with the most recent being its approval in 2021 for the treatment of pediatric patients with moderately to severely active ulcerative colitis.
Humira is currently used in the treatment and management of rheumatoid arthritis, inflammatory bowel disease (Crohn's disease and ulcerative colitis), psoriasis, ankylosing spondylitis, juvenile idiopathic arthritis, and many others. While there are a number of potentially serious side effects and contraindications to its use, Humira's efficacy and benefit to millions of individuals worldwide are likely the reason for it being one of the world's best-selling drugs (per Pharmaceutical Technology).
Here, we'll take a deeper look at the usage, side effects, and dosage of Humira so you'll have a better understanding of this anti-inflammatory medication.
Disease-modifying antirheumatic drugs (DMARDs)
According to StatPearls, disease-modifying anti-rheumatic drugs, also known as DMARDs, are a class of medications that can be used to treat a number of inflammatory diseases. While each DMARD has its own unique mechanism, these drugs work by interfering in critical pathways in the body's inflammatory cascade. DMARDs decrease the function and production of pro-inflammatory cytokines, block signals required for the activation of T-cells, and lower the number of active B-cells. These anti-inflammatory and immunosuppressive effects of DMARDs make them a great choice for decreasing pain and inflammation, reducing or preventing the progression of joint damage and bone erosion, and preserving joint function (per the Cleveland Clinic).
DMARDs can be classified as either traditional or biologic. Traditional DMARDs have been around for a much longer period of time and include the medications hydroxychloroquine (Plaquenil), leflunomide (Arava), methotrexate (Rheumatrex), sulfasalazine (Azulfidine), and azathioprine (Imuran). Biologic DMARDs, on the other hand, are made using modern molecular biology techniques. These typically target more specific molecules in the inflammatory cascade, and are usually given to patients who have not had a good response to traditional DMARDs. Some commonly prescribed biologic DMARDs include Humira, anakinra (Kineret), abatacept (Orencia), etanercept (Enbrel), infliximab (Remicade), and rituximab (Rituxan).
Traditional DMARDs are taken by mouth and can take up to a month to start working. Meanwhile, biologic DMARDs like Humira are given by injection or infusion and begin to take effect after several weeks.
What are monoclonal antibody drugs?
First used in 1986 for the prevention of liver transplant rejection, monoclonal antibodies have become an important treatment option for a variety of diseases (via SingleCare). This includes conditions such as asthma, Crohn's disease, osteoporosis, rheumatoid arthritis, and even COVID-19.
According to StatPearls, monoclonal antibodies are a unique class of proteins that are highly selective for a specific target, commonly referred to as an antigen. Unlike most other medications, monoclonal antibodies are not chemical compounds (per IAVI). Instead, they are based on natural antibodies that are produced by specific immune cells of the body to defend against infection. Monoclonal antibodies work by binding to a specific target, which can range from a surface antigen on a virus to a molecule involved in the immune response.
Humira is one example of a commonly prescribed monoclonal antibody (via American Family Physician). While also being classified as a DMARD, Humira is a recombinant human immunoglobulin G1 monoclonal antibody that "specifically binds and inhibits" the pro-inflammatory cytokine tumor necrosis factor (TNF) alpha. Because TNF alpha is involved in the breakdown of cartilage and bone, monoclonal antibodies that inhibit its activity can be used to treat a multitude of arthritic conditions (per StatPearls). Some other monoclonal antibodies that also target TNF alpha include infliximab (Remicade) and etanercept (Enbrel).
Using Humira to treat rheumatoid arthritis
According to the Mayo Clinic, rheumatoid arthritis is an autoimmune disorder that affects the joints and other body systems. Over time, this disease can damage the bones and joints, resulting in erosion and deformities. Rheumatoid arthritis can also affect the blood vessels, eyes, heart, lungs, and skin.
There are several treatment options for people diagnosed with rheumatoid arthritis (per the Mayo Clinic). The specific medication or regimen is based on symptom severity and how long someone has had the disease. Some common treatment options include non-steroidal anti-inflammatory drugs (NSAIDs), steroids (prednisone), traditional DMARDs, and biologics (Humira, Enbrel, Orencia).
In a 2004 study published in the Annals of the Rheumatic Diseases, scientists looked at the safety and efficacy of Humira monotherapy in patients who did not respond to other DMARDs. After studying 544 patients over 26 weeks, the study concluded that Humira "achieved significant, rapid, and sustained improvements in disease activity and improved physical function and was safe and well tolerated."
According to the Johns Hopkins Arthritis Center, TNF inhibitors such as Humira are part of the American College of Rheumatology recommendations for the treatment of rheumatoid arthritis. From this article on rheumatoid arthritis treatment, "the efficacy of the [TNF inhibitors] is similar across the class in reducing the signs and symptoms of [rheumatoid arthritis], as well as in slowing or halting radiographic damage, when used either as monotherapy or in combination with methotrexate."
Humira may be used to treat inflammatory bowel disease
Inflammatory bowel disease (IBD) is a term used to describe Crohn's disease, ulcerative colitis, and indeterminate colitis, according to Johns Hopkins Medicine. These inflammatory conditions impact around 1.6 million individuals in the United States. IBD is an autoimmune disorder where the body's own immune system attacks healthy cells and tissues in the gastrointestinal tract. While the exact cause is unknown, it likely stems from a variety of genetic, environmental, and immune factors. Some studies have even shown that the gut microbiome in patients with IBD is different from that in healthy individuals, suggesting another possible cause.
Symptoms of IBD tend to depend on the specific type. However, common symptoms include abdominal pain, bloody stools, diarrhea, fever, malnutrition, rectal bleeding, and weight loss. According to the Mayo Clinic, the treatment and management of IBD involves drug therapy, nutritional support, and in severe cases, surgery. Nutritional support centers around preventing excessive weight loss, which is a common complication of IBD. Drug therapy involves the use of aminosalicylates (Delzicol, Colazal), corticosteroids, immunosuppressants (Imuran, Trexall), and biologics (Humira, Remicade, Simponi).
Per the American College of Gastroenterology (ACG) clinical guidelines for treatment of ulcerative colitis in adults, Humira is recommended for patients with moderately to severely active ulcerative colitis. Based on similar ACG guidelines for treatment of Crohn's disease, Humira is also recommended for the treatment of moderate-to-severe Crohn's disease that has failed to respond to conventional therapy.
Can Humira be used to treat psoriasis?
Psoriasis is a skin disorder caused by rapidly dividing skin cells (via WebMD). This rapid growth causes skin in certain parts of the body to build up into itchy, dry, thick, and raised patches covered by white scales (per the American Academy of Dermatology). There are several types of psoriasis, all of which tend to vary in their severity, location, symptoms, and appearance. The most common types include plaque psoriasis (80-90% of cases), guttate psoriasis, inverse psoriasis, pustular psoriasis, erythrodermic psoriasis, nail psoriasis, and psoriatic arthritis.
Treatment and management of psoriasis is based on the Psoriasis Area Severity Index (PASI), which is a measurement tool used to identify the severity of the condition and determine what treatment options are best (via StatPearls). Mild to moderate psoriasis is commonly treated with topical agents. These include moisturizers, coal tar, dithranol, corticosteroids, vitamin D analogs, and retinoids. Ultraviolet light therapy can also be used, and includes PUVA (psoralen with exposure to ultraviolet light) and NBUVB (narrowband UVB light).
Patients who do not respond to topical therapies often switch to immunosuppressant drugs such as methotrexate or cyclosporine. In patients who do not respond well to these, a healthcare provider will likely switch to the use of biologic agents, including Humira. According to the National Psoriasis Foundation, Humira has been approved by the Food and Drug Administration (FDA) for use in adult patients with active psoriatic arthritis and moderate to severe psoriasis.
Humira may be used to treat ankylosing spondylitis
Ankylosing spondylitis is a type of arthritis that causes chronic inflammation of the lower spine and pelvis (via the Cleveland Clinic). Individuals with ankylosing spondylitis experience severe and persistent lower back pain and stiffness. Other symptoms include fatigue, weight loss, abdominal pain, rash, vision changes, and neck pain.
Left untreated, ankylosing spondylitis can result in fusion of the vertebrae (ankylosis), abnormal curvature of the spine, and even cauda equina syndrome (scarring and inflammation of nerves in the lower back). According to the Mayo Clinic, NSAIDs are the most commonly prescribed medications for the treatment of ankylosing spondylitis. They help to relieve pain, inflammation, and joint stiffness. Long-term use, however, can increase the risk of gastrointestinal bleeding. Therefore, TNF inhibitors such as Humira are also commonly prescribed.
Based on a 2018 article published in the journal Open Access Rheumatology, data from multiple clinical trials has proven that Humira is an effective treatment option for patients with ankylosing spondylitis. Patients who took Humira reported improvements in their arthritis, spinal pain, uveitis, psoriasis, and gastrointestinal involvement associated with the disease. This article also found that Humira was a great alternative for those who failed to respond to other biologic agents. Overall, Humira showed an acceptable safety profile and "demonstrated short-term improvement in clinical signs and symptoms, physical function, and health-related quality of life, in patients with active [ankylosing spondylitis]."
Humira and juvenile idiopathic arthritis
Juvenile idiopathic arthritis (JIA) is a type of arthritis that develops in children (per Johns Hopkins Medicine). Similar to rheumatoid arthritis, JIA is an autoimmune disease in which the body's own immune cells attack healthy cells and tissues in the joints and other body systems. While symptoms of JIA can vary from child to child, some of the more commonly experienced symptoms include swollen, stiff, and painful joints, inflammation of the eyes, fatigue, decreased appetite, slow growth, fever, and swollen lymph nodes.
As children often outgrow JIA, treatment is focused on reducing symptoms and making sure that the inflammation does not affect bone development, especially in a young growing child. According to AboutKidsHealth, complications of untreated JIA may include flares, osteoporosis, growth problems, muscle loss, and eye problems.
Common medications used to treat JIA include NSAIDs, corticosteroids that are taken orally or given as an injection into a single affected joint, DMARDs, and biologics. Humira is an effective biologic for children with JIA, according to a study published in the New England Journal of Medicine. Even after two years of continued treatment, children showed a good response to the medication, especially when it came to reducing the number of flares.
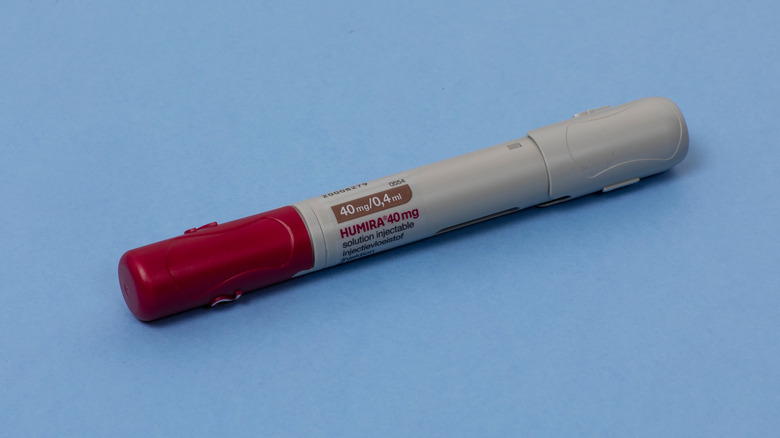
How is Humira administered?
According to the Food and Drug Administration (FDA) Humira Injection Label, Humira is a medication that is administered via subcutaneous injection, a form of injection where a drug is administered into the fatty tissue just underneath the skin (per MedlinePlus). The best areas on the body for a subcutaneous injection are in the upper arms, outer side of the upper thighs, and the belly area.
Humira comes in three dosage forms and strengths. The first is in the form of a single-use pen (often called an "auto-injector"), which contains a 1-milliliter prefilled glass syringe with a fixed needle. This dosage form contains 40 milligrams of the active medication. The other two are in the form of a prefilled glass syringe with a fixed needle. They contain either 20 or 40 milligrams of Humira.
Humira is commonly administered by a trained healthcare worker in a medical facility, such as a doctor's office (via Drugs.com). If given approval by a healthcare provider, a patient can also be allowed to administer the injection themselves in the comfort of their own home. For these individuals, there are several important steps that need to be followed in order to ensure a safe and anxiety-free injection process. These are covered in depth with a healthcare provider before making the transition to at-home administration.
Side effects of Humira
The most common adverse effect following a Humira injection is an injection site reaction (per StatPearls). This can present as redness, itching, pain or swelling. Some other less common but potentially serious side effects may include a fast or irregular heartbeat, swelling of the ankles and feet, fatigue, sudden weight gain, blood in the stool, numbness of the extremities, muscle weakness, vision changes, joint pain, and difficulty swallowing, speaking, and chewing (via Drugs.com).
It is possible to develop an allergic reaction to Humira. This requires immediate medical attention and often presents with difficulty breathing, hives, severe dizziness,and swelling of the face, lips, tongue, or throat. Humira can also cause serious and potentially life-threatening liver disease, especially in patients who have had prior exposure to the hepatitis B virus. Signs and symptoms of liver damage include nausea, vomiting, abdominal pain, appetite loss, dark urine, and yellowing of the eyes and skin (jaundice).
Another serious side effect of Humira includes the worsening or initiation of congestive heart failure, multiple sclerosis, and other neurological diseases.
Some people may develop antibodies to Humira
While Humira itself is a monoclonal antibody, an estimated 5% to 54% of individuals will develop antibodies against the medication (per HCP Live). Also known as anti-drug antibodies, these antibodies produced by the body against Humira can potentially decrease its effectiveness and result in adverse effects.
A study published in the Journal of the American Medical Association showed that "development of anti-drug antibodies is associated with a negative outcome of [Humira] treatment in [rheumatoid arthritis] patients." This study found that patients who developed anti-drug antibodies to Humira had higher rates of disease activity during treatment and had a lower chance of going into remission.
According to the Johns Hopkins Arthritis Center, this phenomenon of anti-drug antibodies is sometimes seen in patients who stop treatment and then re-initiate after an extended period of time. Patients who show a poor response to Humira and have evidence of anti-drug antibodies to Humira may benefit from switching to another biologic agent. This is an area that warrants further investigation.
Humira may cause reactivation of latent tuberculosis
The reactivation of latent tuberculosis is a major risk factor in patients being treated with Humira (per StatPearls). Tuberculosis is a bacteria that can survive within your body without causing you to become ill (via the CDC). Because most people have a functioning immune system, their bodies are able to fight off the bacteria and keep them from growing and causing symptoms. These individuals will not feel sick and will not spread tuberculosis to others. The only sign that these individuals may have tuberculosis is after a positive tuberculosis skin or blood test.
The primary molecule in the human body that keeps tuberculosis from reactivating is TNF (per Clinical & Experimental Immunology). As a TNF alpha inhibitor, Humira can interfere with the immune response and result in the reactivation of latent tuberculosis. For this reason, a healthcare provider will test some for tuberculosis before starting and during treatment with Humira (via Drugs.com).
Can Humira alter your white blood cell and platelet counts?
According to Kaiser Permanente and the European Medicines Agency (EMA) report on Humira, there have been rare cases of bone marrow suppression in certain patients taking Humira, resulting in a condition known as pancytopenia. This condition occurs when the number of red blood cells, white blood cells, and platelets in the blood is below the normal expected count (per the National Cancer Institute). Signs and symptoms include abnormal bleeding, difficulty breathing, easy bruising, fatigue, skin changes, and weakness. The EMA has advised any patients experiencing these symptoms to seek immediate medical attention and for their healthcare providers to consider discontinuing Humira treatment.
There has also been concern over the development of lymphoma, a rare but serious form of cancer that affects the blood and lymphatic systems, in patients taking Humira (per Dermatologic Therapy and the Mayo Clinic). While there is not enough evidence to establish a causal relationship between Humira and lymphoma, there is also not enough data to completely rule it out.
Humira may react with certain medications and vaccines
Humira has "no known severe interactions" with other medications, according to RxList. However, there are some medications which may result in moderate interactions. Some of these include astragalus (a dietary supplement), belatacept (Nulojix), denosumab (Prolia, Xgeva), and hydroxyurea (Hydrea, Droxia).
It is also recommended to avoid live vaccines when taking Humira (per Arthritis Research UK). Live vaccines use a weakened or attenuated form of a virus or bacteria to help prevent disease with that organism (via the CDC). These include the vaccines for measles, mumps, and rubella (MMR), varicella, rotavirus, and influenza (intranasal version only). Some other non-routinely used live vaccines include the adenovirus vaccine, typhoid vaccine, and the Bacille Calmetter-Guerin (BCG) vaccine.
While there are certain circumstances where a live vaccine may be necessary (as in the case of a rubella vaccination in a woman of childbearing age or in the case of a shingles vaccination in an elderly patient), it is best to receive such vaccines before starting treatment with Humira (per Arthritis Research UK). Lastly, the pneumococcal and influenza (intramuscular only) vaccines are safe and recommended for people taking Humira.