Everything You Need To Know Before Getting An Insulin Pump
Chances are you know someone who has diabetes, or you have diabetes yourself. According to the American Diabetes Association, 37.3 million Americans (11.3% of the U.S. population), had diagnosed diabetes in 2019, with an additional 8.5 million adults estimated to be undiagnosed with this chronic condition.
Per the American Diabetes Association, people with type 1 diabetes don't produce insulin at all and need to add insulin to their bodies. People with type 2 diabetes produce insulin, but their bodies don't use it properly. They may be able to control their condition with diet, exercise, and oral medication. When that doesn't do the trick, they too need insulin therapy. There are a variety of ways to get the insulin you need, including with a needle and syringe, an insulin pen, a needle-free jet injection, an injection port, and even by inhaling the insulin (via Healthgrades). Here, we're focusing on yet another approach: the insulin pump.
The prototype for the insulin pump, designed by Dr. Arnold Kadish in 1963, was huge and had to be carried like a backpack (via a paper published in Diabetes Therapy). The technology and design have improved dramatically since then. Today, insulin pumps are widely used to treat both type 1 and type 2 diabetes, and are proven to improve and simplify diabetes management for many people. And don't worry — they're much, much smaller now, too.
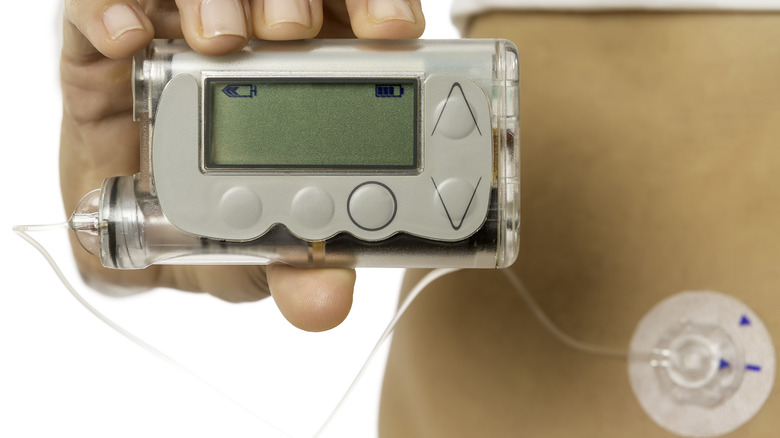
What an insulin pump does and how it works
An insulin pump is a computerized device that's about the size of a smartphone. It's worn outside your body and releases insulin in a steady stream, 24 hours a day, with an extra dose at mealtimes (via WebMD). The steady flow is called basal insulin, and extra doses are called bolus. You program the pump for both basal and bolus doses, and you can adjust the doses depending on what or how much you eat and your activity level. Short-acting and rapid-acting insulin are used in the pumps, not long-acting, and continuous delivery is designed to keep your blood sugar at steady levels.
Traditional insulin pumps deliver insulin through thin plastic tubing into an infusion set, which includes a small tapered tube called a cannula that you insert under your skin, says EndocrineWeb. Angled infusion sets have longer cannulas and are often preferred by athletes, active children, pregnant women, and thin or muscular people. Straight sets have shorter cannulas, making them preferable to people who want to put the infusion set on their arms or in hard-to-reach places, or those who are squeamish of needles. The belly, buttock, or thigh are popular insertion sites because they're most likely to have a layer of fat where you can insert the cannula.
Beyond traditional insulin pumps
Want to skip the tubing used by traditional insulin pumps? The patch pump uses a cannula that you insert under your skin, but the cannula and the insulin delivery chamber are part of a single pod that sits on the skin, attached with an adhesive patch (via the Cleveland Clinic). There's no external tubing, and you can place the patch on your belly or arm. The device is operated with a wireless handheld controller.
There's also a hybrid closed loop insulin pump that links with a second device, called a continuous glucose monitor (CGM), to continuously monitor your blood sugar and automatically adjust the level of insulin based on your body's needs (via Mayo Clinic Health System). Some have tubes and others are tubeless. Some work with certain continuous glucose monitors but not others. And some use a touch screen, while others have physical buttons.
This system, which is approved for use by people with type 1 and type 2 diabetes, is called hybrid because it's not a fully closed loop. It monitors blood sugar and adjusts insulin accordingly, but it requires you to make manual adjustments when you eat a meal or your blood sugar surges for some other reason.
Advantages of insulin pumps
One big advantage of an insulin pump is that it reduces the number of times you need to jab yourself to inject insulin, says Diabetes.co.uk. You just implant the insulin catheter every two or three days and, while that process is more involved than giving yourself an injection, it means you don't need a shot before every meal.
The pump also gives you more flexibility around food and exercise. Decide you want a dessert you hadn't planned on, or agree to a spur-of-the-moment game of tennis? You can easily adjust your pump to provide more or less insulin. Because you can make insulin adjustments throughout the day, insulin pumps are linked to lower risk of severe hypoglycemic (low blood sugar) episodes, and therefore fewer instances of long-term diabetes complications.
You may be a good candidate for an insulin pump if you have trouble controlling your blood glucose levels, or if you're injecting insulin at least four times a day, says Diabetes Care Community.
Disadvantages of insulin pumps
You'll need a certain amount of tech savvy to get your pump set up correctly and to use it properly, so if that's not your strong suit, the insulin pump may not be right for you. Also, you'll need to continue checking your blood sugar several times a day to make sure the pump is working correctly. It can be dangerous and even life-threatening if it's not (via the Cleveland Clinic).
If you don't want people to know you have diabetes, the fact that you need to hide the tubing and pump on your body may be a drawback for you, says WebMD. Plus, pumps can break, tubing can become disconnected, and the insulin pump and pump supplies can be more expensive than just giving yourself insulin injections.
Believe it or not, cybersecurity vulnerability is also a disadvantage of an insulin pump (via Healthcare IT News). It's been discovered that hackers can potentially take control of insulin pumps to manipulate readings or alter medication doses, including overdosing you.
Kids with type 1 diabetes experience significant benefits using the insulin pump
About 283,000 Americans below 20 years of age are said to be diagnosed with diabetes, with approximately 18,200 youths diagnosed annually with type 1 diabetes, and 5,800 with type 2 diabetes (via the American Diabetes Association).
A study in JAMA Network Open found that juvenile insulin pump users who have type 1 diabetes have a lower likelihood of developing diabetic retinopathy (a leading cause of vision loss) than youths who get insulin through multiple daily injections.
Insulin pump users also have fewer hospital admissions due to diabetic ketoacidosis, a complication of diabetes that can lead to diabetic coma or death. "This finding – along with our evidence that pump use protects against retinopathy – suggests clinicians should encourage children and adolescents with type 1 diabetes to use this technology," says retina specialist Roomasa Channa, MD, study co-senior author and assistant professor of ophthalmology and visual sciences at the University of Wisconsin School of Medicine and Public Health (via Johns Hopkins Medicine).
Benefits of an insulin pump if you're pregnant or planning a pregnancy
As your body changes during pregnancy, your blood sugar levels change too. It can also be harder to detect low blood sugar levels, says the American Diabetes Association. At the same time, keeping your blood sugar within targets becomes even more important to ensure your health and the health of your baby. Good blood glucose control helps minimize the risk of miscarriage and birth defects affecting the brain, heart, and spine as the baby's organs are formed (via the Centers for Disease Control and Prevention). It also helps keep your baby from getting too large, because high blood sugar results in the fetus being "overfed."
According to Diabetes Self-Management, a growing number of insulin pump users are women who are pregnant because the pump allows them to achieve and maintain the tight blood glucose control needed for a healthy pregnancy. The pump is most commonly used by women with type 1 diabetes during pregnancy, but it's also used by pregnant women who have type 2 and gestational diabetes.
One advantage of using the insulin pump during pregnancy is that you can make minute adjustments to insulin doses. Additionally, you can change the basal rate of insulin infusion hourly or every half hour. This is especially useful over the course of your pregnancy, as your hormone levels and insulin needs keep changing.
Using an insulin pump does involve some risks
The most common problems with insulin pumps are related to infusion site infections, says Diabetes Education Online. Infections can occur if the infusion set is left in too long, or the injection site isn't prepared carefully. To prevent problems, it's essential that you use the prescribed disinfectant to thoroughly clean your hands, the top of the insulin bottle, the needle, cannula, and infusion set connections (via Information About Diabetes). Getting your infusion set securely attached to your skin will also reduce the risk of infection. If you notice redness, swelling, warmth, or pain at the infusion site, or you get an unexpectedly elevated blood sugar reading, you need to address the issue immediately.
Because insulin pumps are complex devices, stuff can go wrong with them, like batteries failing, tubing getting kinked, insulin reservoirs leaking, needles slipping, or software malfunctioning (via emDocs). Insulin pumps often have reminders and alarms to alert you to problems, but they may alert you too late. And let's not forget the possibility of user error, per an article in Diabetes Care. Anything that results in an interruption of insulin infusion (causing hyperglycemia and ketoacidosis) or delivery of excessive insulin (causing severe hypoglycemia) is a serious and possibly life-threatening issue for insulin pump users.
Concealing your insulin pump involves creativity
It's easy to hook an insulin pump on a waistband or belt, but what if you don't want the whole world to know you have diabetes, and don't want to answer a lot of questions? It's time to get creative, says Hartford HealthCare Institute of Living.
Some clothing companies make clothes specifically for insulin pump users, or garments that have pockets for music players or phones. Other options include sewing a baby's sock to the inside of your clothing to hold the pump, or using an existing pocket to hold the pump and cutting a small hole in the inside of it to insert your pump's tubing. The pump can also be slid inside a trouser sock, clipped to your bra under your arm or between your breasts, or under your spandex shorts or shapewear. If you're wearing the pump next to your skin, stick it in a baby sock first to protect it from sweat and make wearing it more comfortable.
Medtronic offers suggestions specifically for fashion conscious insulin pump users. Wearing a sundress or skirt? You can use a garter or leg strap to conceal your pump. Choose a v-neck one-piece swimsuit that allows you to clip the pump under the front of the suit, or a tankini so you can clip the pump to your bikini-style shorts. And when shopping for formal wear, keep the need for concealing the pump in mind; with some forethought, anything's possible.
Insulin pumps and supplies can be costly
Insulin pumps can cost between $4,500 and $6,500 if you don't have health insurance, says the Academy of Managed Care Pharmacy (via CostHelper Health). Devices with only a few features, such as software that lets you download data to a personal digital assistant, come in at the low end, while a pump with features like continuous glucose monitoring is closer to the high end. Most pumps come with batteries, infusion lines, and syringes, but these products need to be continually replaced, costing an estimated $1,500 a year. And then there's the cost of insulin, which may be about $785 a year without insurance.
If you have health insurance, you can expect to pay a copay and coinsurance rates anywhere from $5 to half the total cost of the pump. The estimate of $5 to 50% of total costs also applies to accessories and insulin if you're insured.
If the cost of a pump is unaffordable for you, talk to your doctor. There may be programs in your area that help people acquire a pump, and some state and federal agencies offer help paying for diabetic supplies.
How to choose an insulin pump
Once you've decided to get an insulin pump, you'll want to carefully research the numerous options, says Kaiser Permanente. Start by asking your healthcare team what they recommend, and check with your insurance company to see which pump brands they cover. Then get online to read up on each type of pump, or ask companies to send you details on their products.
Each insulin pump offers different features, so think about what's important to you and choose accordingly (via Diabetesnet). How easy are the buttons to push, and the screen to read? What reminders and alarms does it have? How much information is stored in the pump's memory, and is it easy to access? And what level of customer service is provided by the manufacturer? You may also want to know how much insulin the pump holds, whether it can work with a continuous glucose monitor, what type of batteries it uses and how long they last, and if the device is water resistant, says Medical News Today.
Your infusion site will require special care
If your insulin pump uses an infusion site, where the insulin goes into your body, you'll want to monitor the site and the infusion set carefully (via Hartford HealthCare Institute of Living). Because the sites are prone to infection, you'll need to learn how to place the catheter correctly, keep the site clean, and replace the infusion set as often as your doctor tells you to, which is usually at least every two or three days.
Moving your infusion site to different locations, such as your hip, your belly, or your thigh helps your tissue continue to be receptive to absorbing insulin. And you need to keep the infusion set at least one inch away from your belly button and any scars you may have, since scar tissue makes it harder for insulin to flow into your tissue.
Getting the infusion set to stay attached to your skin, and not irritate your skin, is another possible challenge of insulin pumps. Products are available to alleviate these problems, as well as to remove any sticky adhesive that may remain when you remove the infusion set. If you find that one type of infusion set doesn't work well for you, try another type. And if your insulin set gets wet during sweaty activities, spraying antiperspirant on the skin around your infusion site before the activity may help solve the problem.
Tips for successfully using of your insulin pump
Once you've chosen your insulin pump, it's time to learn as much as you can about using the device to effectively manage your diabetes and minimize problems (via Diabetes Care Community). If your medical center offers any insulin pump educational sessions, attend one and ask lots of questions. Learn what each of the components do and how to operate them. Read your owner's manual and follow the instructions exactly. If ongoing support and education is available, sign up for that, too. Anything you can learn from the experts will be beneficial.
Get into a routine with your insulin pump. Take your insulin at the same time, every time, such as right before you eat a meal. And keep records of your blood glucose readings, your insulin doses and correction doses, and your physical activities. Reviewing those records daily or at least weekly will give you helpful information on how to better control your blood glucose.
Also, have a alternative plan for insulin delivery in case your insulin pump isn't working for some reason. For example, keep insulin and an insulin pen or syringes handy, just in case. Lastly, visit your healthcare team regularly to make sure the pump is working for you, get help adjusting your doses, and ask all your latest questions.