11 Ways To Improve Insulin Sensitivity
If you're looking for ways to improve insulin sensitivity, then you've come to the right place.
Before we dive in, however, it's helpful to understand that insulin sensitivity refers to the body's sensitivity or responsiveness to the hormone insulin, according to Medical News Today. Insulin itself is a hormone made by specialized cells in the pancreas called beta cells. Insulin's primary role is to reduce blood sugar by allowing the sugars released from the food you eat to enter your cells after digestion. A common analogy used for this is the lock and key analogy. Cells are "locked" but insulin unlocks the "doors" to your cells, allowing sugar and other fuels to pass through. Without functioning insulin, cells cannot receive the energy they need to properly function.
The good news is that insulin sensitivity may be increased through both dietary and lifestyle measures, reducing the risk of type 2 diabetes and other related health complications (per Medical News Today). Here, you will discover many of those helpful measures, as you get to know how to improve your insulin sensitivity.
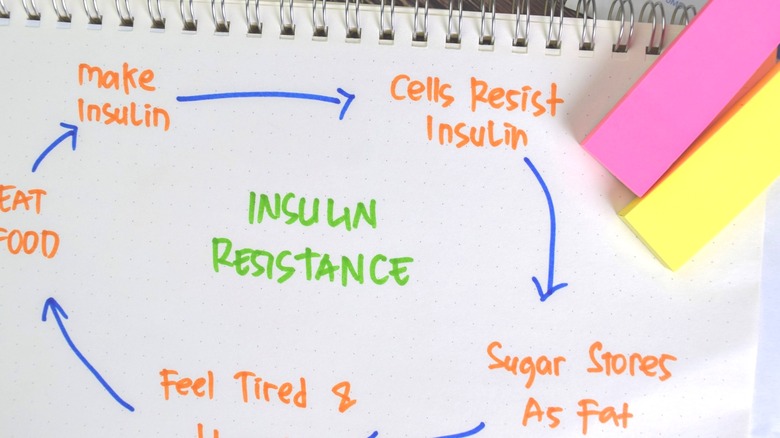
Insulin sensitivity vs. Insulin resistance
A person who is insulin sensitive is highly responsive to insulin, meaning insulin works well and efficiently, so that only small amounts are needed to do the job (per Medical News Today). You want to be insulin sensitive. A person who is not insulin sensitive is conversely referred to as "insulin resistant" — a condition that affects nearly 40% of American adults and puts you at increased risk for developing type two diabetes.
Because the cells do not respond as well to insulin, more is needed to get the job done, leaving a person more vulnerable to type 2 diabetes, a condition marked by high insulin resistance where blood sugar levels become elevated — this contrasts to type 1 diabetes where insulin is simply not produced anymore due autoimmunity (where the body attacks the beta cells in the pancreas so that they no longer function), according to the Cleveland Clinic. Most people with type 2 diabetes produce insulin; the body is just unresponsive to it or no longer able to produce enough, leading to high blood glucose levels.
Practice intermittent fasting
Dietary strategies that reduce blood sugar are often considered among the most effective for improving insulin sensitivity because they address the root of the problem. One strategy that has gained popularity over recent years is intermittent fasting, also known as time-restricted eating. What contrasts intermittent fasting from other types of diets is that it focuses primarily on meal timing rather than calories or specific foods you consume.
According to Healthline, a 2014 review from Translational Research showed that intermittent fasting can greatly improve insulin resistance and reduce high blood sugar levels. Over a study lasting in 8 to 10 weeks in duration, fasting blood sugars decreased by 3-6% in human participants. There was a corresponding drop in fasting insulin after 8 to 10 weeks, a marker of increased insulin sensitivity, by 20-30% as well.
There are many different approaches to intermittent fasting, such as eating in an eight hour window and fasting for 16 hours or eating normally five days a week, followed by restricting calories to one meal (about 500 calories) a couple times a week. If you are interested in trying intermittent fasting, be sure to speak with your doctor first, as it's important with any new diet or exercise program (via Johns Hopkins Medicine).
Eat a lower carb diet
Carbs have the greatest impact on blood sugar and thus insulin levels when compared to the other two energy-yielding macronutrients (proteins and fats), according to Diabetes Forum. This is because all carbs — even starches like bread and pasta — are eventually broken down into sugar. Protein has a small to moderate impact on blood sugar, and fats have almost no effect. For this reason, it makes sense that a lower carb diet results in better glycemic (blood sugar) control and greater insulin sensitivity. According to the site, reducing carb intake (and possibly protein if your intake is too high), helps to reduce circulating insulin levels and insulin resistance. Lower carb diets also tend to increase satiety and reduce overeating and hunger — a double benefit — as overeating worsens insulin resistance.
Reducing insulin levels is important not only because high insulin levels drive insulin resistance, but insulin is also a fat-building hormone, so too much insulin can lead to weight gain, which further compounds insulin resistance. The American Diabetes Association echoes this, stating that blood sugar levels are almost chiefly determined by the balance of carbs you eat and insulin your body produces in response to it.
When you think of a low carb diet, you may think of the popular "keto" diet, which is the strictest form, but even diets that are modestly lower in carbs can show improvements in blood sugar. For example, a 2014 study from Metabolism showed improvements in insulin resistance and weight loss in women with PCOS (an insulin resistance related disorder) with even a modest reduction of carbs from 55% down to 41% of energy intake. While exact definitions are loose, anything from 100 to 150 grams of carbs a day or less is considered a low carb diet, as most Americans consume in far excess of this (per Healthline). The bottom line is that even a modest reduction in carb intake can improve insulin sensitivity.
Focus on whole, unprocessed carbs
By reducing your intake of carbs, especially highly processed carbs that break down quickly into sugar, you can improve your insulin sensitivity. The American Diabetes Association recommends focusing the carbs you do eat on mostly whole, unprocessed carbs that are non-starchy like lettuce, cucumbers, green beans, broccoli, and tomatoes, for instance. Because of their higher fiber content and lower starch content, these tend to have the lowest impact on blood sugar.
Modest amounts of minimally processed higher carb foods like fruits (strawberries, apples, blueberries, and cantaloupe), whole wheat bread and brown rice, peas, beans, and sweet potatoes can also have a place in your diet. Conversely, highly refined, processed carbs like white rice and bread, candy, sugar, fries, pastries, chips, and sweetened beverages should be minimized to the occasional treat, as these can have a substantial impact on blood sugar levels.
For more guidance on how to portion your carb intake, try using the plate method. And if you want a more precise look at your carb consumption, consider looking into carb counting.
Lower your added sugar intake
Among the processed carbs you want to reduce, sugar is at the top of the list (via Health University of Utah). In a recent 2014 report, scientists compared how different types of carbs impact the body, finding that added sugar causes the most significant harm in terms of diabetes risk — this includes both table sugar (sucrose) and fructose, which is concentrated in high fructose corn syrup and added to many processed foods (per the Mayo Clinic).
Only the added sugars posed the greatest risk for diabetes and its related conditions like cardiovascular disease; whereas "whole food" sources of sucrose and fructose like what naturally occurs in fruits and some vegetables posed no risk and was thought to be protective against diabetes. The study goes on to state that the result of this review and other studies has led to the World Health Organization (WHO) to recommend reducing added sugar intake to no more than 5% of total daily caloric needs for adults, about 100 calories (25 grams) or less for most people, citing no need for any added sugars in the diet. Eating this amount of sugar has shown to decrease the prevalence of diabetes and improve insulin resistance, as well as related health outcomes like hyperlipidemia, etc.
Most people know that too much sugar in the diet is unhealthy, but this research directly shows how reducing added sugar intake could translate into lower diabetes rates. Of course, reducing your sugar intake might be easier said than done, but The American Heart Association has many practical tips, such as swapping water or sparkling water for soda or juice, looking at food labels and selecting products with the lowest amount of added sugars or that have no added sugars, and cutting sugar in recipes by ⅓ or ½.
Practice portion control
In addition to the type of foods eaten, blood sugar is also strongly influenced by the total amount of food consumed in a sitting (per the Diabetes Care Community). If too much carbohydrate is consumed at once, blood sugar levels rise sharply, increasing resistance to insulin and weight gain. This is not aided by the fact that portion sizes at restaurants and fast food joints have grown so popular over the decades.
Paying attention to how you feel when you're eating, and making sure you are not overly full is one way to manage portion sizes. But because portion sizes are so large nowadays it can be difficult to gauge what is a "normal" portion. Everyone is different and portions do vary somewhat based on weight, sex, age, activity level, and other factors, so for more personalized guidance, you should consult with a dietitian.
Some of general guidance on portion size from the WebMD Portion Size Guide includes for grains : 1 cup cereal, 1 pancake, or ½ cup cooked rice or pasta. For milk and cheese: 1 cup of yogurt, ½ cup ice cream, or 1 cup milk. For fruits and vegetables include: 1 medium fruit, 1 cup cooked veggies, or 1 cup leafy greens.
Of course, overeating is not a black and white issue. People eat too much for several reasons, and hunger is not always one of them. If you struggle with overeating, try slowing down at meals to give your body time to recognize the sensation of fullness, or get help from a counselor if you feel the amount of food you eat is frequently beyond your control. This may signify a more serious problem like Binge Eating Disorder (BED), which often requires help to treat, explains Healthline.
Lose weight if needed
Research shows that losing as little as 5-7% of your body weight and performing 150 minutes of physical activity per week reduced the risk of developing type 2 diabetes by a whopping 58%, according to the Centers for Disease Control and Prevention (CDC). For adults over the age of 60, it reduced the risk by 71%. Both of these are significant reductions and show the power of weight loss for improving insulin sensitivity and reducing risk of type 2 diabetes.
But why is this? Well, it turns out that body fat distribution is directly related to metabolic complications of obesity such as diabetes, per a 2008 study in the Journal of Endocrinology and Metabolism. Specifically, increased upper body fat around the midsection, also known as visceral fat, is more strongly linked to health complications than fat in the lower body. You may have heard the terms "apple shaped" or "pear shaped" tossed around — people who are more "apple shaped" carry more weight in their midsection which is associated with higher visceral fat storage, a type of fat that surrounds the internal organs. This contrasts with subcutaneous fat which is directly beneath the skin.
Visceral fat is considered "biologically active" and acts similar to an endocrine organ, producing many hormones and substances that have effects on several other tissues (per Harvard Health). Although the fat you can pinch beneath your skin may be annoying, it is not nearly as dangerous as the (fat) layer deep beneath the abdominal wall.
Reduce visceral fat
So why else is visceral fat particularly dangerous? According to a 2008 study in the Journal of Endocrinology and Metabolism, "An upper body/visceral fat distribution in obesity is closely linked with metabolic complications, whereas increased lower body fat is independently predictive of reduced cardiovascular risk."
These are the same fats associated with clogged arteries, heart attacks, and insulin resistance. Visceral fat also releases many inflammatory chemicals into the blood which may impair liver metabolism. Perhaps, most notable is that even at a normal body mass index (BMI), weight stored in the upper body is still associated with poorer health outcomes. More fats are also delivered from the liver to the upper body, which can lead to health problems, including insulin resistance as the liver becomes "full" with fat and a less efficient reservoir for storing excess sugar.
Exactly why high visceral fat leads to insulin resistance and diabetes is not known, but one hypothesis is that the free fatty acids that visceral fat produces interfere with the function of the insulin-producing cells (beta cells) of the pancreas. Due to this strong link between body fat distribution and health, experts now recommend that men maintain a waistline no greater than 40 inches and women no greater than 35 inches, according to WebMD. If your waist measures more than this, consider talking to your doctor about weight-management tools. Some of the strategies (intermittent fasting, carb counting, portion control) mentioned earlier for insulin resistance, can also aid weight loss.
You can also consider joining the National Diabetes Prevention Program. Unlike most dietary programs, even a decade after following the DPP program, participants were a third less likely to develop type 2 diabetes than those who didn't participate.
Do resistance training
While your carbohydrate intake plays the biggest role in determining blood sugar and thus insulin resistance susceptibility (via the American Diabetes Association), being physically active does have an important role also. Resistance training in particular seems to be beneficial for insulin resistance, according to a 2019 study published in Diabetes and Control. When ten overweight men engaged in three sessions of resistance exercise for six weeks, they experienced a stunning 16% increase in insulin sensitivity. The study concluded that resistance training may help to improve insulin sensitivity and reduce risk of type two diabetes.
But why is this? In a 2016 review, Diabetes & Metabolism states that when muscles become depleted of their stored glycogen (starch) from either aerobic or resistance training, there is a greater capacity to store excess sugar, which improves insulin sensitivity (via Everyday Health). But a newer 2018 study out of the American Journal of Physiology: Endocrinology and Metabolism went even further, stating that resistance exercise increases the effects of a key protein involved in blood sugar absorption known as APPL1.
It was demonstrated in rats that exercise increases the effectiveness of APPL1 by activating four different signaling pathways that turn on during resistance training and increase APPL1 expression. Although the study was done in rats and doesn't prove this happens in humans, this (and further) research could help to explain the improved glucose intake in muscle following regular exercise. The CDC recommends two days of muscle resistance exercise like weight training or body weight exercises in the Physical Activity Guidelines for Americans.
Exercise 150 minutes a week
Most of the exercise you do should be aerobic — with current recommendations advising 150 minutes of moderate intensity or 75 minutes of vigorous intensity aerobic exercise per week, according to the CDC. Aerobic exercise gets your heart rate up for a sustained period of time and makes you breathe harder but can usually be maintained for a while before you have to take a break.
The Cleveland Clinic, according to a 2017 study, explains that regular exercise has many benefits related to insulin resistance such as activating a nutrient-sensing enzyme known as AMPK, which encourages glucose intake in skeletal muscle, increasing the density of muscle mitochondria (which burn up carbs), and increase the function of proteins that aid in insulin signaling. Exercise also reduces fat mass and inflammation, which is linked to type 2 diabetes and heart disease. The study adds that just a week of aerobic exercise training improved liver insulin sensitivity as well, even in the absence of restricted calorie intake.
Three months of regular aerobic exercise also improved beta cell function (cells that make insulin) in people with type 2 diabetes who had at least some function left. Shorter duration but higher intensity exercises like HIIT and CrossFit also improved beta cell function in people with type 2 diabetes. And Diabetes Care says, "In individuals with type 2 diabetes, regular training reduces A1C, triglycerides, blood pressure, and insulin resistance."
Monitor your blood sugar and A1C
Having your fasting blood sugar and A1C checked regularly is a good idea if you are worried about insulin resistance or diabetes. A1C is also known as the hemoglobin A1C test or HBA1C test and calculates your average blood sugar over the past three months. This provides a deeper snapshot into how you're managing your blood sugar over time as opposed to a one-time snapshot seen with fasting blood sugar tests (via the CDC). Like fasting blood sugar, A1C is commonly used to diagnose prediabetes or diabetes as well as the severity.
A1C actually measures a protein found on your red blood cells called hemoglobin. Since blood cells live an average of three months before dying (per UC Santa Barbara), the amount of sugar attached to your hemoglobin can be used to estimate your average blood sugar levels over the past few months.
An A1C test is recommended every three years for adults over 45 or anyone under that age with risk factors for insulin resistance such as being overweight, having a family history of diabetes, being sedentary, or coming from a demographic more prone to type 2 diabetes, such as being African American or Hispanic, according to the CDC. If your A1C is high, you should repeat this test according to your doctor, or at least once a year. A1C ranges are as follows:
Normal is less than 5.7%, pre-diabetes is 5.7-6.4%, and diabetes is 6.5% and over.
Monitor your insulin levels
The only downside to the fasting blood sugar and A1C tests is that they can only diagnose prediabetes or diabetes — but insulin resistance happens before A1C starts to rise. This is because for many years the body can usually compensate for higher blood sugar levels by raising insulin to match it — a condition called compensatory hyperinsulinemia, according to Metabolism Journal. As long as your body makes enough insulin to keep your blood sugar levels stable, you will have normal levels but could still be at risk for pre and type 2 diabetes.
Unfortunately, there is not a specific test for insulin resistance alone, but some providers are recommending having fasting insulin levels checked, though this test is not routine and you will likely have to request it. A higher fasting insulin can show that the body is struggling to keep up with rising blood sugar levels, which is an early warning sign for impending prediabetes. While the standard definitions consider high insulin to be 25 units or more, some experts point out that this number is simply an average of the American population, who are largely insulin resistant, and is not a good number to aim for (per Medscape). Insulin levels lower than eight (ideally, four to five) means the pancreas isn't having to work too hard to keep blood sugar levels managed, according to Knew Health. Another type of test that indirectly measures insulin resistance is the HOMA-IR test, according to Self Decode.
There are also some interesting physical signs associated with hyperinsulinemia such as dark, velvety patches in folds of skin (under arms and neck come to mind) called acanthosis nigricans, excessive hunger, sugar cravings, and great difficulty losing weight as excess insulin promotes fat storage (per Healthline and the Mayo Clinic). However, not everyone has symptoms.
If you have higher than desired fasting insulin levels and/or symptoms of hyperinsulinemia, consider speaking with your doctor and taking some of the preventive steps discussed in this article.