Medical Conditions That Can Cause Loss Of Taste (That Aren't Covid)
The last few days, you've been feeling crummy. Your nose alternates between being stuffy and running like a sieve. You have a bit of chest congestion and a cough that isn't going away. You take a sip of your favorite latte and notice you barely taste it. Whether you've lost your taste completely or are experiencing altered taste loss, you might assume that you have COVID since it's a common symptom (per research published in PLOS Medicine). But a recent negative test has you scrambling for what could be causing your loss of taste.
According to the Cleveland Clinic, a loss of taste is called ageusia in medical terms. This condition makes it impossible or difficult for people to perceive the most common tastes of sweet, bitter, salty, and sour. There is no age limit on who the taste loss affects, and it can come from several different conditions like bacteria and viral infections, gum disease, diabetes, Sjogren's syndrome, head injuries, and Parkinson's disease. Learn more about how these medical conditions might lead to a loss of taste, as well as treatment options that can help you get back to enjoying the flavors of your food.
Sinus infections affect your taste buds
Your taste has been off for a few days, and you feel considerable pressure under your eyes. Coupled with a runny nose (and possibly congestion), you're most likely dealing with a sinus infection. According to the American College of Allergy, Asthma & Immunology (ACAAI), sinusitis, the medical term for a sinus infection, affects about 31 million people in the U.S. alone. It's also responsible for more than 16 million doctor's visits.
Sinusitis is typically caused by a bacterial infection that has found a home in your sinus cavity and started multiplying. Inflammation irritates the nasal cavity, filling the sinus cavities with fluid. In addition to feeling intense facial pressure, you can also have a fever. The Cleveland Clinic notes that it's not just bacteria that can cause sinusitis; fungal infections, viruses, and allergies can also be to blame.
Sinusitis doesn't always cause you to lose your sense of smell and taste. Still, it can happen because the infection irritates the lining of the nerve and throat, per Capitol Breathe Free Sinus & Allergy Centers. It's also more common for those with a viral sinus infection to lose their sense of taste.
Influenza messes with your sense of taste
You can get the flu any time of the year, but it's more common to succumb to it during flu season. A range of influenza viruses cause the flu. An infection typically leaves you feeling feverish, sore, and exhausted. You can also have a scratchy throat, cough, and runny nose, according to the Centers for Disease Control and Prevention (CDC). Since the flu is an upper respiratory infection, inflammation in the lining of the nose and throat is common. Per the CDC, about 8% of the population gets the flu yearly.
Since the flu can mess with the lining of your nose and throat, it can potentially affect your sense of smell and taste. You can lose your sense of taste completely, but you'll likely have a reduced sense of taste, or things might taste weird. The Taste and Smell Clinic notes that about 1% of those with the virus might succumb to a taste or smell dysfunction. This typically clears up once the virus has moved out of their body, and they begin to get healthy. However, it can stay on for those with a latent viral response. Treatment for the flu includes antiviral medication, rest, and hydration.
Common cold congestion hinders flavor
A cold isn't nearly as debilitating as the flu, but it can be annoying. Caused by several different viruses, the common cold lasts for about a week and causes stuffy nose, sore throat, sneezing, and fatigue (via the Mayo Clinic). You might even run a low-grade fever, but it doesn't knock you down like the flu or COVID-19 can. Since it causes inflammation in the nasal passages and throat, it can lead to a loss of taste and smell.
"Other viral infections, such as colds, can result in a loss of smell and taste," explains Dr. Melissa McBrien, an otolaryngologist (via Beaumont). "Sometimes this is just for the length of the cold when the nose is blocked, but other times the lack of smell can last weeks to months." The range of the loss of your taste depends on the severity of your loss of smell. FEMA Flavor noted that tasting is an experience of both the taste buds and smell, so it can make things taste off when the smell is affected.
Common colds don't have a cure, but you can get over-the-counter treatments to help alleviate some of the more annoying symptoms like runny nose.
Strep throat leads to a loss of taste
If you've ever experienced strep throat in your lifetime, you know it can make you feel horrible. It not only makes swallowing feel like your mouth is full of glass, but also leaves you with a fever and fatigue. Your tonsils also swell and get white patches. Strep throat is caused by a bacteria known as group A streptococcus. While anyone can get strep throat, Penn Medicine states that it's most common in children and teens. It gets transmitted via person-to-person contact and can spread among family members.
Strep throat causes severe swelling in the throat and tonsils, making swallowing a chore. So, it should be no surprise that it can affect your taste buds. Mount Sinai notes that a loss of appetite and abnormal taste can be among other symptoms of the disease. Diagnosis requires taking a strep test to find out if strep is present. The infection is treated with a round of antibiotics for around ten days. It can also be helpful to gargle with salt water and throat lozenges.
Gum disease inflammation limits taste
Your taste buds being affected by the cold and flu makes sense, since they cause inflammation of or near your taste receptors. But gum disease can also limit the ability of your taste buds due to chronic inflammation.
Periodontal (gum) disease generally comes from poor tooth care, which is why your dentist emphasizes the importance of brushing and flossing. Over time, plaque develops and hardens, leading to tartar. When left untreated, it can cause swollen and bleeding gums, according to the National Institute of Dental and Craniofacial Research. Chewing can become a nightmare, and your teeth might even start to loosen.
Per Modern Dentistry of Shrewsbury, as gum disease starts to take hold, patients might notice a bitter or sour taste in their mouth that has nothing to do with their eating. Brushing teeth or chewing gum can help, but the taste can return within a few hours. Reflections Dental also notes that the increased inflammation can cause your ability to taste at all to decrease. Treatment for the condition depends on the severity of the disease and infection. Brushing and flossing your teeth and visiting the dentist can help prevent this disease from taking hold.
Diabetes slowly limits taste
Patients with diabetes can also experience an alteration or complete loss of sense of taste, known as a diabetic tongue. Diabetes is a chronic condition where the pancreas doesn't release insulin correctly. Therefore, your blood can get flooded with sugar, causing your blood sugar to skyrocket, according to the CDC. Aside from a loss of taste or altered taste, other symptoms of diabetes are weight loss, fatigue, weakness, and slow healing (via the Journal of Family Medicine and Primary Care).
The why behind the loss of taste goes back to the brain and glycemic control, per research published in Nutrients. Those who have diabetes that is poorly controlled can be at a higher risk for gum disease. They can also get sensory neuropathy that can alter their taste perception. However, those with controlled diabetes can also succumb to the loss of taste due to the effect diabetes has on the body. This is particularly true for tasting sweet foods.
Sjogren's syndrome impairs sense of taste
When you're fighting a cold or bacterial infection, your immune system sends out its soldiers — white blood cells — to defend your body. However, your immune system can also malfunction, which happens when it attacks healthy cells rather than invaders. Sjogren's syndrome is an autoimmune disorder where the glands that produce moisture are seen as the bad guys, so your body starts to fight them. Due to the malfunction in your system, those with Sjogren's syndrome have a problem producing tears and saliva. This can cause your mouth to feel chalky and your eyes to feel irritated, according to WebMD.
Research in Nutrients showed that patients with Sjogren's syndrome may also experience a loss of taste, burning in the mouth, and halitosis. Those with this condition lack the protective effects of saliva, which can lead to gum disease and mouth infections, per the National Institute of Arthritis and Musculoskeletal and Skin Diseases. It can also cause inflammation in the sensitive lining of the mouth. Treatment works by providing artificial saliva and tears to make patients feel more comfortable.
Taste is affected by allergies
Allergies can find their roots in our immune system. Some individuals are predisposed to be allergic to particular substances, like pollen. This can lead to various symptoms, like watery eyes or a runny nose. According to the ACAAI, when your body encounters a substance that it sees as a foreign invader, it overreacts by producing antibodies, which trigger the symptoms of your allergic reaction. More research is required before the mechanism behind the triggering of allergies can be completely understood.
Those with severe allergies can have a loss of smell, which can lead to a loss of taste. Prevention notes that the nerves that allow you to smell are cut off due to inflammation. When you lose your sense of smell, this negatively impacts your sense of taste. So, someone with allergies might lose both their sense of smell and taste. It can also lead to more severe conditions like sinusitis.
Treatment for allergies requires antihistamines, which can negate your body's overzealous reaction to the allergen. You might also need additional treatments like steroids (via the Mayo Clinic).
Dry mouth can decrease taste
You don't realize how essential moisture is for your mouth and taste until you experience a dry mouth. This can leave your mouth feeling gritty and thick. When you have dry mouth, your mouth doesn't produce enough saliva, according to NHS Inform. Dehydration is one of the most common reasons for dry mouth; you can't make spit when you don't have enough fluid in your body. However, it's not the only reason why dry mouth happens. You might also experience dry mouth due to medication, nerve damage, tobacco use, and cancer therapy.
Dry mouth can lead to an altered sense of taste and a complete loss of taste. When it's caused by dehydration, getting fluids into your system as soon as possible is imperative. Other causes of dry mouth might require more invasive treatments. The Mayo Clinic notes you might need to switch medications or use an over-the-counter or prescribed medicine to provide you with artificial saliva in the form of a wash or moisturizer. You might also be prescribed medications to help encourage the production of saliva. Dry mouth can also lead to gum and tooth problems, so it's essential to treat it urgently.
Head injuries can cause taste disorders
Many may not be aware that hitting one's head or nose could cause their sense of taste to go. The Brain Injury Association explained that taste and smell can be affected differently during a brain injury. Sufferers might experience distorted taste or a total loss of taste. They might also have a consistent bad taste in their mouth.
Research in the Journal of Neurology, Neurosurgery & Psychiatry showed that patients might experience problems with taste perception even after seemingly minimal head trauma. The loss of taste might not happen immediately after the injury, making it hard to pinpoint the cause. Some individuals might have an average taste reaction for months afterward, only to suddenly experience a loss. For some individuals, taste distortions can be devastating, and can make eating difficult. In this case, medication (i.e., gabapentin) might be needed to help alleviate the problem, per Flint Rehab.
You can also try other ways to stimulate your taste receptors. For example, you might try sucking on ice to improve your sense of taste. Experiment with different textures when the taste is gone or distorted from a head injury. Taste enhancers can also work for some people.
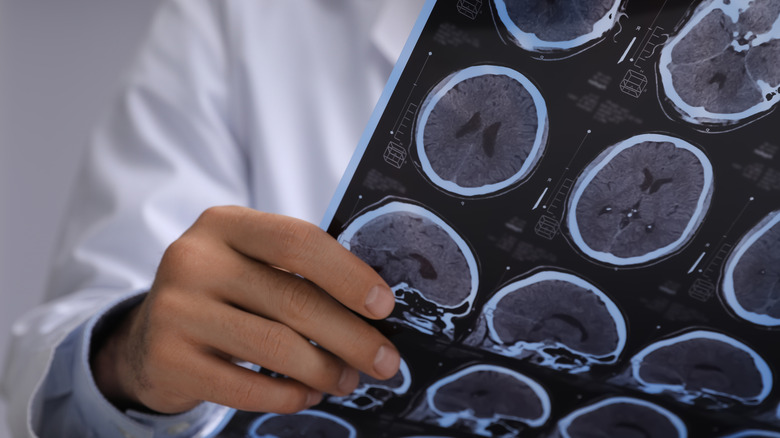
A symptom of multiple sclerosis is a loss of taste
Neurological disorders can affect different areas of your brain, including the area that handles taste and smell. Multiple sclerosis (MS) is an autoimmune disease where the body mistakenly attacks the myelin sheath surrounding the brain and spine. Over time, damage to the nerve fibers leads to muscle weakness, numbness, loss of balance, fatigue, and muscle spasms, according to the Cleveland Clinic. While rare, it can also lead to a loss of taste.
A study by the Multiple Sclerosis Trust examined MS patients' sense of taste. The results showed that patients with more lesions in their brain scans had a more significant loss of taste and taste distortions. The study also found that salty tastes were the ones with the most difficulty to ascertain, with 32% of the participants struggling. On the flip side, bitter flavors were the easiest ones for MS patients to taste. Additionally, men appeared to have more difficulty than women identifying tastes, because the latter have more taste buds.
While there isn't a cure for MS, treatments are available to help reduce flare-ups and attacks. Patients can also take part in counseling and rehabilitation.
Parkinson's disease and a loss of taste
Apart from progressive difficulties with walking and talking, Parkinson's disease also leads to behavioral changes, memory difficulties, and fatigue, according to the National Institute on Aging.
The cause of Parkinson's disease isn't completely understood yet, but experts know that the cells in the brain responsible for movement become impaired and die. In addition, they lose the nerve endings that generate norepinephrine, the hormone and neurotransmitter that affects a person's circadian rhythm and is involved in their fight-or-flight response. Evidence suggests that both genetic and environmental factors can lead to the disease.
Research published in the Journal of Neurology showed a possible link between the combined loss of smell and taste and the risk of Parkinson's disease development. Per Parkinson's News Today, taste and smell loss happen due to changes in brain connectivity. Additionally, patients may demonstrate altered smell and taste sensitivity when Parkinson's is in its initial and moderate phases.